Living independently with a disability isn’t about going it alone. It’s about having the choice and control to live life on your own terms, with a trusted support team backing you up every step of the way. This isn't just a distant dream; it's a completely achievable reality with the right plan and support.
Charting Your Course to Independent Living
Stepping into the world of independent living is exciting, but let's be honest, it can also feel a bit overwhelming. This guide is here to break it all down, giving you the knowledge and confidence to take charge.
True independence is built on a foundation of support you can rely on. It’s about creating a life that works for you. We’ll walk through everything you need, from figuring out your specific needs to building that perfect care team. For NDIS participants in Sydney, this is all about turning your goals into a solid, actionable plan.

Defining Your Version of Independence
First things first: what does independence actually look like for you? This vision is the bedrock of your entire plan, so it’s worth spending some real time on.
Think about the specifics:
- Choice in daily routines: You decide when you wake up, what’s for breakfast, and how you spend your day. For example, independence could mean being able to sleep in until 10 a.m. on weekends, rather than sticking to a facility's rigid schedule.
- Control over your environment: You have the final say on who comes into your home and how your space is set up to work for you. This could be as simple as choosing the music you listen to in the afternoon or deciding you want a quiet evening without visitors.
- Access to your community: You should have the freedom to pop out to the shops, visit friends, or get to appointments safely and easily. A practical example is having the support needed to go to your local footy game every Saturday.
- Management of your health: This means working with a clinical team that genuinely respects your decisions and supports your health goals from the comfort of your own home. For instance, if you need daily insulin injections, you decide the most convenient time for a nurse to visit, fitting it around your work or study schedule.
For many NDIS participants, one of the biggest roadblocks is finding suitable housing. The current housing shortage is a serious issue affecting people's safety and autonomy. Nationwide, the demand for Specialist Disability Accommodation (SDA) sits at 25,274. Here in NSW, 8,027 people have SDA funding, but a staggering 3,012 are still waiting for a place to call home. You can dig into these numbers in the NDIS housing data report.
These figures show just how vital in-home nursing services are. They bridge a critical gap, providing support for complex needs like seizure monitoring or dysphagia management. This allows people to thrive at home, even while navigating the challenging housing market.
Independence is built on a foundation of reliable support. It’s knowing you have a skilled team ready to assist with complex health needs, giving you the confidence to pursue your goals without compromising your well-being.
Navigating this journey is a lot easier when you know what resources are out there. To learn more, check out our guide on how Independent Living Centres can assist you.
Designing Your Personalised Independence Blueprint
Before you can build a life of greater independence, you need a clear blueprint. This isn't just a to-do list; it's a detailed, personal map of what living independently with a disability looks like for you. It’s all about defining your goals, figuring out the specific supports you need to get there, and putting it all down on paper.
This blueprint becomes your personal guide. It makes your vision clear and acts as a powerful tool in NDIS planning meetings, helping to ensure your funding actually aligns with your real-life ambitions. Think of it as a living document—one that should grow and change right alongside you.
From Big Dreams to Actionable Steps
One of the biggest hurdles is thinking only in broad strokes. A goal like, "I want more community access," is a fantastic starting point, but it's too vague to be practical for planning. The real trick is to break down those big dreams into small, manageable, and supportable actions.
Let’s think about 'Alex,' who requires ventilation support but dreams of joining a weekly art class. That's his big-picture goal. Now, let's break it down into concrete steps:
- Transport: Alex will need a wheelchair-accessible vehicle and a support worker who can help with the journey from his home to the class and back again.
- Clinical Support: To be safe and comfortable, a trained nurse or a highly skilled support worker must be with him during the class to monitor his ventilation equipment.
- Scheduling: His current care schedule needs to be adjusted to free up a specific afternoon each week. This means coordinating with his whole support team.
By breaking it down like this, Alex moves from a simple wish to a concrete plan. He now has specific, fundable support items to discuss in his NDIS meeting, making his goal much more achievable.
Mapping Out Your Daily Life and Needs
To create a truly effective blueprint, you have to do a bit of a deep dive into your own daily life. Think through every part of your day, from the moment you wake up to when you go to bed. This detailed approach is the best way to make sure no support need, big or small, gets overlooked.
Start by asking yourself some practical questions across different areas of your life:
- Personal Care: What specific help do you need with showering, dressing, or grooming? For instance, do you need someone for 30 minutes in the morning to help with buttons and zippers, or full assistance with showering?
- Mealtime Management: Do you need a hand with grocery shopping or preparing meals? Do you require specialised support due to dysphagia, like having someone prepare texture-modified meals?
- Health and Medical Needs: What clinical supports are non-negotiable? This could be anything from a nurse visiting twice daily for medication management and catheter care to weekly support for complex wound dressing.
- Community and Social Goals: What activities do you really want to do? For example, "I want to go to the library once a week." What support is needed to make that happen safely—like a support worker to assist with transport and carrying books?
Documenting these details gives you clarity and also shows your NDIS planner and support coordinator that you have a well-considered plan. For anyone with ongoing health issues, knowing how to manage them is a core part of this. You can find more on effective strategies in our guide on chronic condition management.
The following checklist can help you start mapping out your needs and goals. Take your time with it—it's a great tool for self-reflection and for preparing for NDIS planning conversations.
Independence Plan Self-Assessment Checklist
Use this checklist to identify and document your specific support needs and goals across different areas of your life.
| Life Domain | Current Support Level (Low/Medium/High) | My Independence Goal | Specific Supports Needed (e.g., Nurse for injectables, Support Worker for meals) |
|---|---|---|---|
| Personal Care (e.g., showering, dressing) | |||
| Meal Management (e.g., shopping, cooking) | |||
| Health & Clinical Needs (e.g., medication) | |||
| Home & Household Tasks (e.g., cleaning) | |||
| Community & Social Life (e.g., hobbies) | |||
| Appointments & Transport | |||
| Communication & Technology | |||
| Other (Specify) |
Once you’ve filled this out, you’ll have a much clearer picture of where you are now and where you want to go. It's the foundation for building your support network.
Thinking Beyond Traditional Models
Your blueprint should reflect the life you want to live, not one that's forced to fit into a pre-existing box. For some people, this means looking at options like Individualised Living Arrangements (ILAs), which offer a real path to independence outside of traditional group homes.
An effective independence plan is built on choice and control. It’s about having the right support, in the right place, at the right time, allowing you to live the life you envision for yourself.
ILAs are such a powerful model for person-centred support. In fact, research shows that if just 500 more people transitioned to ILAs each year, it could save the NDIS $260 million over five years. Despite this, only about 520 NDIS participants currently live this way. For people in Sydney with complex needs like ventilation support or epilepsy care, a provider can integrate skilled nursing care right into an ILA, customising support to fit individual goals perfectly. You can discover more insights about this promising housing model and its benefits.
Securing NDIS Funding for In-Home Support
Getting a handle on your National Disability Insurance Scheme (NDIS) funding is the first real step towards a more independent life. The whole system can feel a bit overwhelming at first, but once you get the hang of the main ideas, you’ll be in a much better position to ask for what you truly need to live where—and how—you want.
Let's cut through the jargon. We're going to break down the most important funding types and show you how to talk about your needs in a way that makes sense, ensuring your NDIS plan actually helps you reach your goals.
Understanding the Key NDIS Funding Buckets
Two of the most crucial funding categories for living on your own are Supported Independent Living (SIL) and Specialist Disability Accommodation (SDA). They often get mixed up, but they pay for completely different things. It’s vital to know the difference.
Specialist Disability Accommodation (SDA): Think of this as the funding for the bricks and mortar. SDA covers the cost of living in a house that's been specially built or modified to make life easier and safer for someone with significant functional impairment. A practical example is an apartment with widened doorways, a ceiling hoist, and a fully accessible bathroom.
Supported Independent Living (SIL): This is the funding for the people who support you inside that home. It pays for personal care, help with everyday tasks, and the supervision you need to live as independently as you can. For instance, SIL funding could cover a support worker who helps you with meal preparation every evening and provides overnight assistance.
There’s a common myth that SIL is only for group homes, but that’s just not true. You can absolutely use your SIL funding to arrange 24/7 support right in your own home. For many people, knowing this is a total game-changer, giving them ultimate control over their living situation.
How to Ask for What You Need in Planning Meetings
Your NDIS planning meeting is your chance to really be heard. This is where you draw a straight line from your personal goals to the supports you need to achieve them. The trick to a good meeting? Be specific, be clear, and always talk about your goals. If you're too vague, you'll likely end up with a plan that doesn't quite cover what you need.
So, instead of just saying, "I need some help at home," you’ve got to frame your requests around what you want to achieve.
Here’s a real-world example:
Let's say your goal is to enrol in a part-time TAFE course. To make that happen, you need things at home to be running smoothly.
- Don't say: "I need more support in the mornings."
- Instead, try this: "My goal is to attend my TAFE course three days a week. To do that, I need two hours of personal care support each of those mornings to help me with showering and getting dressed. This will make sure I can get to class on time and ready to learn."
See the difference? This approach directly links the support you're asking for (personal care) to a clear, measurable goal (attending TAFE). You can learn more about how NDIS funding covers these essential daily supports in our guide on Assistance with Daily Life.
The most powerful way to make your case is to tie every single support request back to one of your personal goals. This turns your plan from a simple list of services into a genuine roadmap for your life.
When you speak this way, it helps your NDIS planner understand why the support is necessary, making it far more likely to be included. Walk into that meeting with your independence plan clear in your mind and be ready to share concrete examples from your day-to-day life.
The Power of SIL Funding for Real Independence
For anyone with significant support needs wanting to live on their own, SIL funding is often the cornerstone. Even though the NDIS is designed to help people do just that, many still find themselves in group homes.
Across Australia, about 33,500 people receive SIL funding. Its impact is huge—the average plan size jumps from $313,000 without SIL to $608,000 with it. That figure really shows the level of personalised support it makes possible.
The need is massive. In New South Wales alone, 8,027 people have funding for SDA, but 3,012 of them are still waiting for a suitable home to become available. This just underscores how critical it is to have providers who can deliver person-centred, in-home nursing and support, letting people live with dignity in a home of their choosing.
You Don't Have to Do It Alone: Getting a Support Coordinator
Navigating all of this can be tough, but you don't have to go it alone. A good Support Coordinator can be your most valuable ally on this journey. Their entire job is to help you understand your NDIS plan and put it into action.
A great Support Coordinator will:
- Connect you with the right providers: They have a network of trusted services and can help you find the perfect match for both your clinical and personal needs. For example, if you require peg feeding support, they will know which local providers have nurses specifically trained in this area.
- Help you manage your budget: They know the ins and outs of the funding categories and will make sure you’re getting the most out of every dollar to hit your goals.
- Get you ready for plan reviews: They'll help you pull together all the reports and evidence you need to show that your plan is still working for you as your needs change.
Think of them as your strategic partner. By working closely with a Support Coordinator, you can build a solid support system that truly empowers you to live life on your own terms.
Assembling Your Expert In-Home Care Team
Once you have your NDIS funding sorted, the next big step is building your support team. This isn’t just about finding people to help out; it’s about bringing together a skilled, compassionate team who truly understand your goals and respect your home as your own personal space.
This team is the bedrock for living safely and with dignity on your own terms. It’s often a mix of professionals, each playing a different but connected role. Knowing who does what is absolutely key to getting the right support in place from the get-go.
Defining the Roles in Your Care Team
Your in-home team might include several specialists, all depending on what you need. A registered nurse, for example, is essential for any clinical tasks that need proper medical training. This could be anything from complex wound care and managing feeding tubes to administering specialised injections.
Support workers, on the other hand, are your go-to experts for help with daily living. They can assist with personal care, preparing meals, or providing the support you need to get out and about in the community. For instance, a support worker might accompany you to the grocery store, while a registered nurse is the one who later helps you manage your insulin pump. It's common to have a team that includes both, working together seamlessly to cover all your bases.
Let's look at a real-world example. Imagine ‘Maria,’ who is getting ready to go home from the hospital with a new enteral feeding tube. For her, living independently really hinges on having a well-coordinated team.
A quality provider will work directly with Maria’s hospital discharge team, her GP, and her dietitian. This makes her transition home not just safe, but also smooth and a lot less stressful. Her registered nurse will handle the clinical side of her feeding plan, while her support workers will help with daily tasks, all working from a single, unified care plan. It’s this kind of collaboration that stops crucial details from falling through the cracks.
The infographic below shows just how significant the investment is through the NDIS to support participants with complex needs at home.
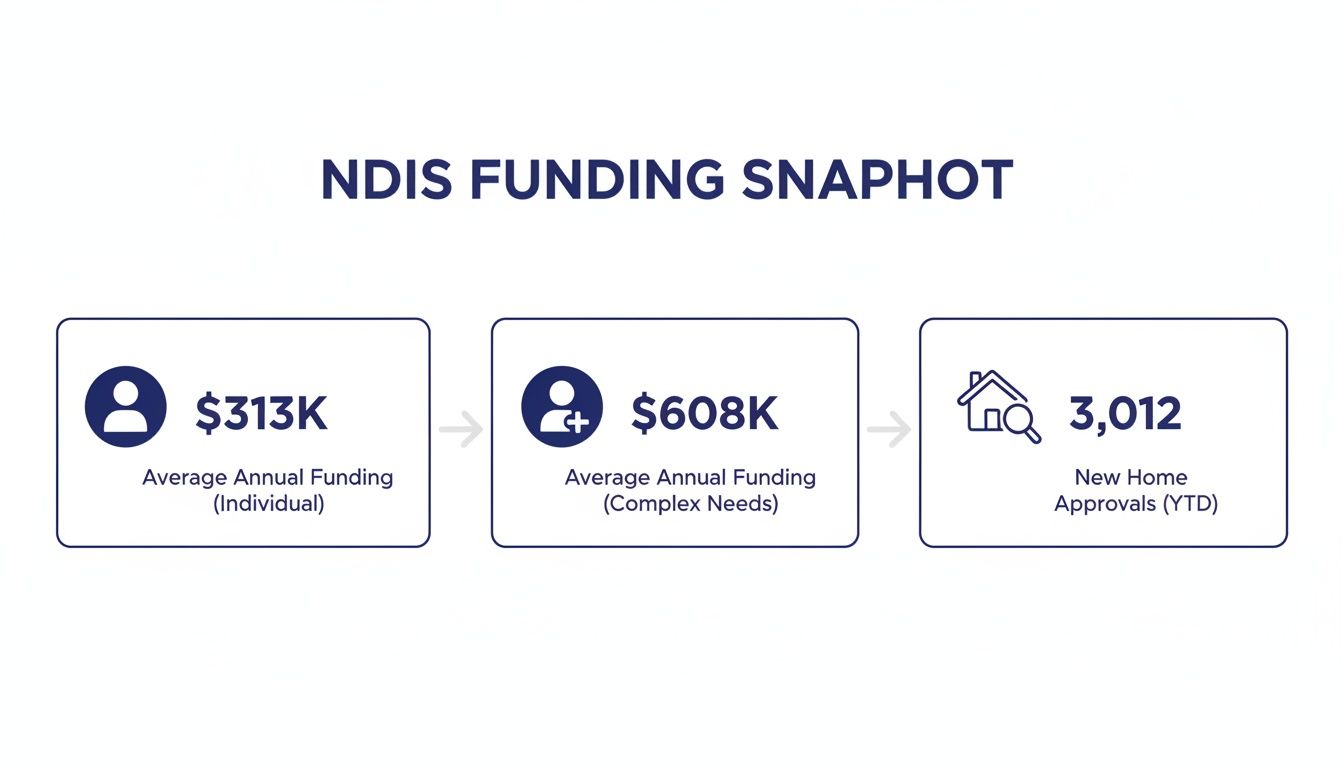
These numbers show there's a real financial commitment from the NDIS to fund the kind of comprehensive support teams people need to live safely and independently.
Finding the Right Provider for You
Choosing a provider is one of the most personal and important decisions you’ll make. This is the organisation that will be sending people into your home, so you have to feel confident in their skills, their professionalism, and their respect for your independence. To get it right, you need to ask the right questions.
When you're meeting with potential providers, think of it as an interview—because that’s exactly what it is. You are hiring them to help you live your life your way.
Your home is your sanctuary. The right care team respects this, not just by providing skilled support, but by honouring your space, your choices, and your dignity at all times.
To help you make a confident choice, I’ve put together a checklist of crucial questions to ask. A provider you can trust will have clear, straightforward answers for every single one. If you'd like some more background, our overview of home care services in Sydney can give you additional context.
Essential Questions to Ask Potential Providers
Use this list to guide your conversations and see how different organisations stack up.
- Qualifications and Training: "What specific training and qualifications do your nurses and support workers have, especially for my needs (e.g., ventilation support, complex wound care)?"
- Team Selection: "How much say will I have in choosing the actual support workers and nurses who will be part of my team?"
- Emergency Planning: "What's your protocol for emergencies? If my regular nurse is sick, what’s the backup plan to make sure my care isn’t interrupted?"
- Communication: "How will the team communicate with me, my family, and my GP? Who is my main point of contact if I have a question or a problem?"
- Experience: "Can you give me some examples of how you've supported other people with needs similar to mine to live independently?"
- Respecting Your Home: "What policies do you have to make sure your staff respect my privacy, my home, and my personal preferences?"
Taking the time to ask these questions will give you a much clearer picture of how a provider really operates. It will help you find a partner who is not just clinically skilled, but genuinely committed to supporting your vision of living independently.
Adapting Your Home for Safety and Accessibility
Your home should be your sanctuary—a place where you feel comfortable, safe, and empowered, not a space filled with daily hurdles. When independence is the goal, the right environment makes all the difference. This goes beyond just having support workers; it means taking a good, hard look at the physical space you live in.
With some smart home modifications and the right assistive technology (AT), your home can truly support your independence. These changes don’t have to be massive, overwhelming projects. They can be anything from small, practical tweaks to larger structural alterations, and with the right advice, many can be funded through your NDIS plan.

Simple Fixes vs. Complex Projects
It helps to think about home modifications on a spectrum. The NDIS actually categorises them to make sure the support you get lines up with what you need.
Simple Modifications are usually low-cost and don’t involve knocking down walls. These are the quick wins that can immediately boost your safety and make life easier.
- Installing grab rails: Placing these in the bathroom, hallways, or next to your bed gives you that extra bit of stability right where you need it.
- Lever-style tap handles: If you have limited hand strength, these are a game-changer compared to fiddly round knobs.
- Non-slip flooring: A few non-slip strips in the shower or some well-placed mats can make a world of difference in preventing falls.
Complex Modifications, on the other hand, are the bigger jobs that involve structural changes. These will need building permits, in-depth assessments, and a higher level of funding.
- Building a ramp: This is a fundamental change for wheelchair access, opening up your connection to the community.
- Widening doorways: Standard doorways are often too narrow for wheelchairs. Widening them is a serious job but essential for free movement.
- Creating a fully accessible bathroom: This could mean installing a roll-in shower, lowering the sink, or repositioning the toilet for proper access.
The Power of Assistive Technology in Daily Life
Beyond the structural stuff, assistive technology (AT) offers some incredible tools to make daily life smoother. AT is really just any device or system that helps you do something you might otherwise find difficult. The possibilities here are huge and always evolving.
Just think about how AT can simplify your day-to-day:
- Smart Home Devices: Using your voice to control lights, heating, or even lock the doors gives you control without needing to move around. A practical example is saying "Hey Google, turn on the bedroom light" when you can't reach the switch.
- Medication Dispensers: These automated gadgets can remind you to take your meds and dispense the right dose, taking one more worry off your plate. This is perfect for someone who takes multiple medications at different times of the day.
- Communication Aids: From simple picture boards to high-tech speech-generating devices, these tools ensure you can always express yourself and stay connected. For instance, a person who is non-verbal could use a tablet with specialised software to order a coffee at their local cafe.
Why an Occupational Therapist is Your Best Ally
So, how do you figure out exactly what you need and, crucially, how to get it funded? This is where an Occupational Therapist (OT) becomes an indispensable part of your team. An OT is a highly skilled allied health professional who is an expert at looking at you, your abilities, and your environment.
An OT doesn't just see a disability; they see your life. Their job is to find practical ways to bridge the gap between what you can do and what you want to do, making your home work for you.
An OT will visit your home and do a full assessment, watching how you handle your daily routines. They’ll pinpoint the barriers and recommend real-world solutions. For instance, they might notice you struggle to get pots from a high cupboard and recommend installing pull-down shelving. Most importantly, they will write a detailed report with clinical reasons for every single modification or piece of AT they recommend. This report is the key piece of evidence you’ll need to secure NDIS funding.
Getting this professional input is vital. You can find out more about connecting with these experts in our guide to allied health services. By working with an OT, you’re not just changing a few things at home—you’re creating a personalised space designed for safety, accessibility, and genuine independence.
Common Questions About Independent Living
Thinking about living on your own is exciting, but it’s natural to have a few questions pop up. It’s a big step! Let's walk through some of the most common things people ask when they're starting to plan.
How Do I Start the Conversation About Moving Out With My Family?
This is often one of the trickiest parts. The best way to approach this chat is as a team, not as an announcement they have to accept. Wanting more independence is a really positive thing, and it helps to frame it that way from the start.
Before you sit down with them, try to have a basic plan sketched out. This shows you’ve really thought it through. For example, you could say, "I've been researching accessible apartments in the area, and I've found a support provider who can offer the overnight nursing care I need." This shifts the idea from a dream to something real and achievable.
The key is to reassure your family that this isn't about pushing them away. It's about building a future where you're in the driver's seat. A great way to do this is to invite them to be part of the journey. Ask if they’d come with you to meet a Support Coordinator or help interview potential care providers. This makes them feel included and respected, turning a tough talk into a collaborative effort.
What Happens If My Health Needs Change Unexpectedly?
This is a really important and valid worry. It’s exactly why a good plan needs to be flexible. The NDIS is built for this – your plan can be reviewed if your circumstances change, making sure your funding keeps up with what you need.
But more than that, this is where having a responsive clinical team makes all the difference. Your support team shouldn’t just be there to react to problems.
A dynamic care plan isn't just about responding to emergencies; it's about anticipating needs. Proactive clinical oversight from registered nurses ensures that small changes in your health are identified and managed before they become bigger problems.
For instance, if you have a pressure sore that is getting worse, a proactive nurse will not only treat it but also immediately contact your GP and an OT to assess your mattress and seating. This kind of proactive care is all about keeping you safe and healthy, giving both you and your family genuine peace of mind.
Can I Choose My Own Support Workers and Nurses?
Yes, you absolutely can. Choice and control are at the heart of the NDIS, and that definitely includes who comes into your home to support you. You should always be the one making the final call.
The right personality fit is so important for building trust. After all, these are the people you'll be working with every day. We always encourage our clients to be deeply involved in choosing their team.
This can look like a few different things:
- Reviewing Profiles: We can share the experience and qualifications of potential nurses and support workers.
- Holding Interviews: You can meet them, either online or in person, to see if you get along. You could ask practical questions like, "How would you help me prepare my favourite meal?" to see how they respond.
- Setting Up a Trial Period: It can be a good idea to arrange a few introductory shifts to make sure everyone works well together in practice.
Your opinion isn't just a "nice to have"—it's essential. We believe that building a team you feel comfortable and safe with is a non-negotiable part of living independently.
Is It Possible to Live Alone If I Need 24/7 Support?
Yes, it is entirely possible, and many people with round-the-clock needs live very successfully on their own. This is where Supported Independent Living (SIL) funding is so critical. While many people think of SIL for group homes, it can absolutely be used to fund a dedicated team of carers in your own home.
This model uses a carefully coordinated roster of support workers and nurses. They work in shifts to make sure someone is always there to meet your needs. We specialise in this kind of high-acuity care, including complex supports like:
- Overnight tracheostomy management
- Continuous ventilation support
- Active seizure monitoring and response
For example, a person with complex epilepsy might have an 'active' overnight shift, where a trained support worker is awake and present all night to provide immediate assistance if a seizure occurs. We work closely with you, your family, and your Support Coordinator to design a 24/7 roster that covers all your clinical needs and personal routines. This ensures your safety is the top priority while empowering you to live in your own space, not a facility. It’s a powerful example of how the right support makes living independently with a disability a reality for people with even the most complex health needs.
At Core Nursing Solutions Pty Ltd, we believe that expert, person-centred care is the key to unlocking true independence. Our multidisciplinary team of registered nurses and support workers is dedicated to providing the high-acuity support you need to live safely and confidently in your own home. To learn how we can help you build your ideal in-home care team, visit us at our website.

Pingback: Home Health Care: Person‑Centred for Better Well‑Being