Managing a chronic illness is about so much more than just sticking to a medication schedule. It’s a complete, hands-on strategy for living your best life, even with a long-term health condition. Think of it like looking after a classic car; it needs a skilled crew, consistent maintenance, and a clear roadmap to keep it running beautifully. For example, just as a mechanic checks the oil and tunes the engine, a good chronic illness management plan involves regular blood sugar checks for diabetes or breathing exercises for COPD.
A Practical Guide to Managing Chronic Illness at Home

Living with a chronic illness can often feel like a full-time job. It’s a constant juggle of appointments, treatments, and keeping an eye on your own health. For NDIS participants and their families, figuring out how to manage all of this at home is the key to holding onto independence and quality of life.
The reality is, long-term health conditions are becoming more and more common.
In Australia, almost half the population—50% of people across all ages—is now living with one or more chronic conditions. That’s a big jump from 42% back in 2007-08. This trend really shines a light on the growing need for properly structured, in-home support.
This guide is here to break down what it really means to manage a chronic illness. We'll show you how to build a support system that actually works for you, moving beyond just reacting to symptoms and toward a coordinated approach that puts you firmly in the driver’s seat.
The Core Pillars of At-Home Care
Good chronic illness management isn’t built on one single thing. Instead, it rests on a few essential pillars that all work together. When these are in place, they create a strong foundation for your health and wellbeing.
- Empowered Self-Management: This is all about giving you and your family the knowledge and confidence you need. For example, a person with asthma learns to use their peak flow meter correctly and understands what the readings mean for their action plan.
- Expert Clinical Support: This brings skilled nursing care right to your doorstep for more complex needs. A practical example is a nurse visiting to administer intravenous antibiotics, saving a trip to the hospital.
- Coordinated Care Planning: This piece makes sure your whole support team—from your GP to your physiotherapist—is on the same page. For instance, the nurse shares notes on wound healing with the GP, who can then adjust medication accordingly.
- Proactive Safety Monitoring: This is about spotting and managing risks before they turn into emergencies. A great example is a nurse identifying that a loose rug is a fall hazard for someone with mobility issues and suggesting it be removed.
A well-structured plan for chronic illness management doesn't just treat a condition; it supports the person. It’s about integrating medical needs with personal life goals to foster independence and dignity.
This comprehensive approach allows NDIS participants in Sydney and Wollondilly to get high-quality clinical support without leaving the comfort and familiarity of home.
By understanding these pillars, you can navigate your NDIS plan more effectively and advocate for the services that will make a real difference. Our team at Core Nursing Solutions specialises in bringing these elements together. We offer expert disability home care services that empower you to take charge of your health journey.
Putting You in the Driver's Seat with Self-Management

True chronic illness management is about so much more than just following a list of instructions. It’s about you playing an active part in your own health journey. This is where self-management comes in.
This is easily the most empowering part of your care. It shifts you from being a passenger to becoming the captain of your own ship. Your clinical team? They’re your expert navigators, there to guide you.
The whole approach is built on a foundation of knowledge and confidence. It means really understanding your condition, learning to recognise your body’s unique signals, and feeling equipped to make smart decisions every single day. The goal is to build the skills you and your family need to handle daily health challenges with real autonomy.
What Does Self-Management Look Like in Action?
Self-management isn't a single action. Instead, it’s a collection of daily habits and skills that put you back in control. It's about connecting the dots between what you do and how you feel, turning abstract medical advice into something tangible you can use in your real life.
Here are a few practical examples of how NDIS participants put self-management into practice:
- Understanding Symptoms: For someone with epilepsy, this might involve a family member learning to spot the subtle pre-seizure signs, often called auras. This allows them to help create a safe space before a seizure begins, which dramatically reduces the risk of injury.
- Managing Medications: It could be an individual learning to give themselves their own insulin injections. Over time, they start to understand how different doses affect their energy levels, adjusting their routine with guidance from their community nurse.
- Making Lifestyle Choices: A participant with diabetes might start a food and blood sugar diary. By tracking what they eat and seeing the direct impact on their glucose readings, they feel empowered to make smarter dietary choices that help stabilise their condition.
These actions build a powerful sense of independence and are absolutely crucial for improving your health in the long run. Learning these skills can be a key part of your journey, and you can explore more on how structured support helps with our guide on assistance with daily life for NDIS participants.
Building Confidence and Key Skills
Developing self-management skills doesn't happen overnight. It’s a gradual process of learning and building up your confidence with the right support from your care team. The focus is on giving you practical tools to manage your health proactively, not just reactively.
Think of it like learning to drive a car. At first, you have an instructor (your nurse or GP) sitting right beside you, offering guidance at every turn. But over time, you gain the confidence to handle familiar roads on your own. Eventually, you feel prepared to handle unexpected traffic or detours with skill.
Self-management transforms chronic illness care from a passive experience into an active partnership. It's about ensuring you have the knowledge, skills, and confidence to be the primary decision-maker in your day-to-day health.
A supportive environment is absolutely essential for this to work. Your clinical team’s role isn’t just to provide treatment, but to educate, encourage, and empower you. They are there to answer your questions, celebrate your progress, and help you troubleshoot challenges along the way. For example, a nurse might create a visual guide to help a participant remember the steps for cleaning their catheter, building their confidence through practice.
Bringing High-Level Nursing Care Into Your Home
Managing a chronic illness often goes beyond daily self-care. Sometimes, it involves complex clinical support that many people think is only available in a hospital. The good news is, specialised nursing services can be delivered safely and effectively right in your home. This approach dramatically reduces the need for stressful hospital visits. Ultimately, it ensures you receive consistent, high-quality medical attention in a place where you feel most comfortable.
Bringing this level of care home means a registered nurse performs critical tasks with skill and precision. This gives you peace of mind and often leads to better health outcomes. It’s about transforming your living space into a safe, supported environment where your clinical needs are met without turning your life upside down.
Demystifying Complex Clinical Services
When we talk about in-home nursing, we’re referring to skilled medical procedures that require a registered nurse’s expertise and training. Let's break down what some of these services actually look like day-to-day.
Take complex wound care. This is so much more than just changing a bandage. A trained nurse assesses chronic ulcers or surgical wounds, understanding the delicate stages of healing. They use advanced dressings and techniques to prevent infection and help you recover faster. For example, a nurse might manage a wound VAC (Vacuum-Assisted Closure) device to help a persistent leg ulcer finally heal.
Similarly, ventilation support at home might sound full-on, but it's a common and safe practice with the right oversight. A nurse makes sure equipment like CPAP or BiPAP machines are working correctly. They also check that masks fit properly to prevent pressure sores, ensuring your breathing is consistently supported. Expert management like this helps prevent respiratory issues and greatly improves sleep quality.
Practical Examples of In-Home Nursing
To give you a clearer picture, let's look at a few scenarios. Each one shows how a skilled nurse from Core Nursing Solutions performs a task that is fundamental to managing a chronic illness well.
- Enteral Feeding Management: For someone unable to eat normally, a nurse manages their PEG tube or another feeding device. They make sure the formula is given correctly and keep the site clean to prevent infection. They also know how to troubleshoot any blockages, making sure vital nutrition is delivered safely.
- Catheter Care: A nurse can manage indwelling or suprapubic catheters. They perform sterile changes to prevent urinary tract infections, which are a common risk. In addition, they monitor output and make sure the system is functioning without any problems.
- Tracheostomy Management: This involves highly specialised care. A nurse performs suctioning to keep the airway clear, cleans the site, and does routine tube changes. This constant, expert attention is crucial for safe breathing and preventing serious infections.
- Medication Administration: This goes far beyond simple reminders. A registered nurse can administer complex medications like insulin or blood thinner injections. As a result, you know the correct dosage is given at exactly the right time.
"Bringing hospital-grade nursing into the home isn’t just about convenience; it’s about continuity. It allows for a deeper therapeutic relationship between the nurse and the participant, leading to more personalised and proactive care that can prevent complications before they start."
This approach means that even with significant health challenges, you can maintain your independence and stay connected to your community. To learn more about how this works, you can find valuable insights in our articles on in-home nursing.
At-Home Clinical Nursing Services for Chronic Conditions
To pull it all together, the table below gives a quick overview of common at-home nursing services. It shows the conditions they often support and the direct benefits for NDIS participants.
| Clinical Service | Commonly Supports Conditions Like | Key Benefit for Participants |
|---|---|---|
| Complex Wound Care | Diabetic ulcers, pressure sores, post-surgical wounds | Faster healing, reduced infection risk, and avoids frequent clinic visits. |
| Ventilation Support | Sleep apnoea, COPD, neuromuscular disorders | Improved breathing and sleep, reduced risk of respiratory distress, and greater energy levels. |
| Catheter Care | Spinal cord injuries, multiple sclerosis, urinary retention | Prevention of infections, increased comfort and dignity, and greater confidence in daily activities. |
| Enteral Feeding | Stroke, dysphagia, neurological conditions | Ensures safe and adequate nutrition, prevents aspiration, and supports overall health. |
| Tracheostomy Care | Respiratory failure, airway obstructions | Maintains a clear airway for safe breathing, reduces infection risk, and enables communication. |
By having access to these services at home, you and your family can manage complex health needs with confidence. The presence of a registered nurse provides not only expert medical care but also invaluable education and support. This empowers you to become an active partner in your own health journey.
How to Build a Coordinated and Effective Care Plan
A great care plan is the master blueprint for your health journey. It’s a detailed, written strategy that makes sure everyone on your support team—from you and your family to your GP and allied health professionals—is working towards the same goals.
Without one, managing a chronic illness can feel disjointed and overwhelming. Important details can easily fall through the cracks.
Think of it like building a house. You wouldn't start without a detailed plan showing where every wall, window, and wire goes. A care plan does the same for your health. It maps out every piece of your support so the final result is strong, stable, and exactly what you envisioned for your life.
This unified approach turns a collection of separate appointments and treatments into a single, cohesive strategy designed around you.
Key Components of a Strong Care Plan
A truly effective care plan is more than just a list of medications. It's a living document that gives clarity, direction, and peace of mind to everyone involved. To make sure nothing gets missed, it has to be detailed and cover all the bases.
A robust plan should always include these essential components:
- Clear Health Goals: These are specific, measurable goals you set with your care team. Instead of a vague goal like "feel better," a practical goal might be, "be able to walk to the local shops twice a week without significant pain within three months."
- Detailed Medication List: This includes all prescribed medications, over-the-counter drugs, and supplements. For instance, it would list "Metformin 500mg, twice daily with food, for Type 2 Diabetes," not just "diabetes pill."
- Scheduled Interventions: The plan outlines all regular clinical tasks. For instance, it will note "change wound dressing on left heel every Monday, Wednesday, and Friday" or "physiotherapy session every Tuesday at 10 am."
- Emergency Protocols: This section clearly states what to do in an emergency. It lists key contacts, details specific warning signs to watch for (like seizure triggers or signs of respiratory distress), and provides step-by-step instructions for caregivers. A good example would be: "If blood sugar drops below 4.0 mmol/L, administer glucose gel and re-test in 15 minutes."
This diagram shows how different at-home clinical nursing services like wound care, ventilation support, and catheter care form the core of a hands-on clinical care strategy.
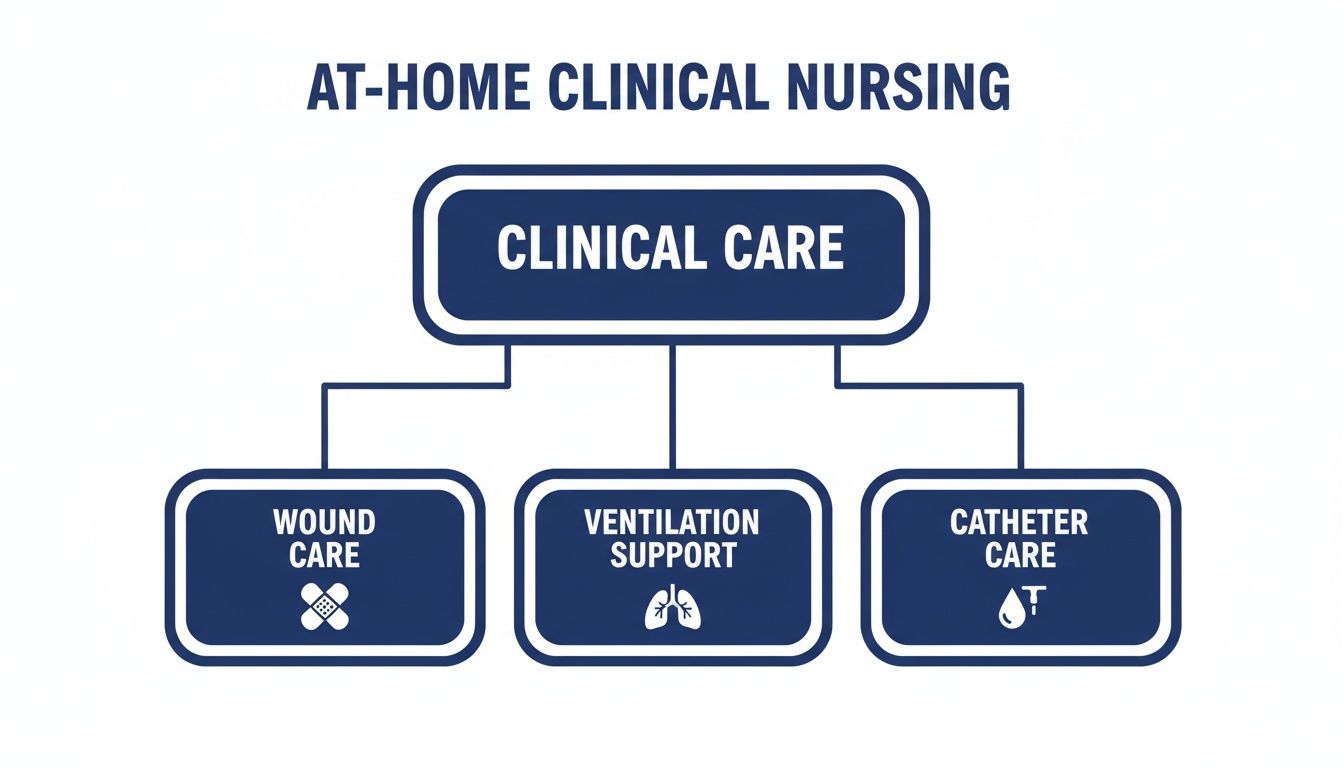
Each element represents a specialised skill that is integrated into a participant's care plan to manage specific health needs proactively at home.
Bringing the Team Together
The real power of a care plan is its ability to coordinate your entire support network. Providers like Core Nursing Solutions act as a central hub, ensuring seamless communication between everyone. This teamwork is crucial for preventing gaps in care and making sure your support adapts as your needs change.
Australia actually excels in this area, ranking in the top 5 OECD countries for quality and coordination of primary care. However, recent data shows that people with multiple conditions often report lower confidence in self-management, highlighting the vital need for proactive, home-based support.
A coordinated care plan ensures that the right hand always knows what the left hand is doing. It’s the central source of truth that aligns every decision and action with your long-term health objectives.
Let's look at a practical example. Imagine a person with mobility challenges and dysphagia (difficulty swallowing).
- The Nurse manages their enteral feeding tube to ensure they get safe nutrition.
- The Physiotherapist works on building their strength and balance.
- The GP regularly reviews their overall health and medication.
- The Family helps with daily exercises and monitors for any changes.
The care plan links all these efforts together. The nurse's notes on nutritional intake inform the physio's exercise plan, and the GP uses reports from both to make decisions about medication. This teamwork ensures every aspect of the person’s health is supported. For a deeper look into the agreements that underpin this structured care, check out this helpful NDIS service agreement template.
Creating a Safe Environment for Complex Health Needs

Great in-home care is built on a solid foundation of safety. This means going way beyond basic precautions and creating an environment where health risks are managed before they turn into emergencies.
For NDIS participants with complex health needs, a safe home is the bedrock of successful chronic illness management. It’s about having a skilled professional who can spot subtle but critical changes and act on them straight away. This gives you and your family real peace of mind.
This proactive approach is exactly what skilled nurses bring into your home. They are trained to see the whole picture, connecting small signs to potential risks. In short, they create a space where you can receive care with confidence.
Identifying and Managing Risks Proactively
A huge part of a nurse's role is to be a health detective, constantly looking for clues that might signal a problem. This isn't about waiting for a crisis; it's about stopping one from ever happening. Their clinical training lets them pick up on minor shifts that others might miss.
For instance, if someone is on a ventilator, a nurse will listen for tiny changes in breathing patterns or notice a slight increase in fatigue. These subtle cues could be the first signs of a respiratory infection, allowing for a quick intervention with the GP before it gets serious.
It's a similar story when caring for a complex wound. A nurse doesn’t just change the dressing. They look for faint redness around the edges, a minor change in smell, or a tiny increase in fluid. Catching these early signs of infection is critical to preventing sepsis and avoiding a trip to the hospital.
Practical Strategies for Home Safety
Creating a safe setting involves specific, practical actions tailored to your unique health needs. It’s about adjusting the environment and setting up routines that minimise known risks. This is always a team effort between the nurse, the participant, and their family.
Here are a few real-world examples of how this works:
- Creating a Seizure-Safe Space: For a person with epilepsy, a nurse assesses the home for potential hazards. This could mean recommending padded corners for sharp furniture, making sure beds are low to the ground with mats beside them, and developing a clear seizure management plan that everyone in the house understands.
- Implementing a Bowel Care Routine: For someone with a spinal cord injury, a consistent bowel care routine is essential for preventing serious issues like impaction or autonomic dysreflexia. A nurse establishes a regular schedule and technique, tracks the results, and tweaks the plan as needed to maintain health and dignity.
- Preventing Falls and Pressure Sores: A nurse will assess mobility and skin integrity at every single visit. They might reposition someone in their bed or chair regularly, check that walkways are clear of clutter, and teach family members how to safely help with transfers.
"Proactive risk management in the home is the quiet work that prevents the loud emergencies. It's the constant vigilance and small adjustments that make a profound difference in a person's long-term health and wellbeing."
These strategies aren’t just about clinical tasks; they are about building a secure foundation for daily life. As a result, participants can focus on their goals and live more independently, knowing that an expert is always looking out for their safety.
How to Fund Nursing Care with Your NDIS Plan
Figuring out how to use your NDIS plan for clinical nursing care can seem a bit tricky at first. But, once you know how it works, you unlock the door to getting the right support at home. A well-prepared request can make all the difference.
The first step is always to connect the nursing support you need directly to your disability-related health needs. Your NDIS plan is there to fund supports that help you manage these specific needs, live more independently, and be part of your community.
Aligning Nursing with NDIS Support Categories
You won’t find a category labelled "clinical nursing" in your plan. Instead, these services are funded through broader support areas. Knowing where they fit is the key to making a successful request.
The most common place to fund in-home nursing is under Improved Daily Living. This category is designed for therapeutic supports that help you build skills and independence. Skilled nursing care, which often includes training for you and your family, is a perfect match here. For example, a nurse teaching a participant how to self-administer insulin falls under building skills.
Another important category is Assistance with Daily Life, especially for the day-to-day support that helps you manage personal care safely. An example would be a nurse assisting with catheter changes as part of a daily routine.
Proving Care is Reasonable and Necessary
The heart of any NDIS funding request is showing that the support is 'reasonable and necessary'. This just means you need to provide clear evidence that explains why skilled nursing is essential for you. Your goal is to build a strong case showing these services are a valuable and effective way to manage your health.
To do this, you’ll want to gather a few key documents:
- Reports from your GP or specialist: This is your most powerful piece of evidence. The report should detail your chronic condition and explain exactly why a registered nurse is needed for things like tracheostomy care or managing a complex wound.
- Assessments from allied health professionals: A report from an occupational therapist or physiotherapist adds extra weight. For instance, an OT report might state that nursing support is needed to manage a feeding tube, which in turn allows the participant to engage in therapy.
- Your own impact statement: Don't underestimate the power of your own words. Describe how having a nurse at home helps you live safely and, just as importantly, helps you avoid trips to the hospital. For example: "Having a nurse manage my wound care at home meant I did not have to be readmitted to hospital last month when I showed early signs of infection."
When you can clearly explain that expert wound care at home prevents costly and disruptive hospital stays, you’re showing its value. This frames your request as a reasonable and necessary support.
Coordinated in-home care is more important than ever, with nearly 40% of Australians now living with more than one chronic condition. Using NDIS funding for in-home nursing is a smart way to manage complex needs and reduce hospitalisations. You can discover more about this trend from this insightful report on multimorbidity.
By getting the right evidence together and framing your request well, you can confidently ask for the support you need to manage your health at home. For more detail on how these services are structured, you might find our guide on the cost of home care services helpful.
Got Questions? We've Got Answers
Stepping into the world of in-home care and the NDIS can feel like learning a new language. We get it. That's why we've put together some of the most common questions we hear, with clear, straightforward answers.
Our goal is to help you and your family feel confident and informed about managing chronic illness at home.
How Do I Know If I'm Eligible for In-Home Nursing in My NDIS Plan?
Getting in-home nursing covered by your NDIS plan all comes down to showing it’s ‘reasonable and necessary’ for your specific disability-related health needs. It isn’t automatically included, so you need to build a strong case with the right evidence.
You’ll need reports from your GP or specialists that clearly outline your condition. These documents need to explain exactly why you need a skilled nurse—for things like complex wound care, medication injections, or catheter changes—to live safely at home. For example, a letter from a respiratory specialist is crucial for proving the need for at-home ventilation support.
We can help you and your support coordinator pull together the right documentation, making sure your request clearly shows why this support is essential for you.
What's the Difference Between a Support Worker and a Registered Nurse?
Think of a support worker and a registered nurse (RN) as two distinct but equally vital players on your care team. Your support worker is your go-to for help with daily living, personal care, and getting out into the community, always working under supervision. For instance, they can help you with grocery shopping or meal preparation.
An RN, on the other hand, brings advanced clinical training to the table. They handle the complex medical tasks that require a higher level of skill, like giving injections, managing ventilators, or changing catheters.
For managing a chronic illness well, you often need both working together. The RN provides the expert clinical oversight and handles medical procedures, while the support worker delivers that crucial, hands-on help for daily life.
What Happens to My Care Plan If My Condition Changes?
A care plan should never be a set-and-forget document; it’s a living guide that evolves with you. Our nurses are constantly checking in, assessing how you’re doing, and keeping the lines of communication open with you, your family, and your GP.
If your health changes or you decide on new goals, your nurse will immediately get the ball rolling on a plan review. For example, if a participant's mobility improves after physiotherapy, the nurse might coordinate with the team to reduce fall-prevention measures and set a new goal, like walking to the letterbox.
This teamwork ensures your supports are always perfectly in sync with your current needs. It keeps your care safe, relevant, and effective as you move along your health journey.
At Core Nursing Solutions Pty Ltd, our experienced team of registered nurses and support workers delivers expert, person-centred care to NDIS participants across Sydney and Wollondilly. We work with you to create a safe and supportive home environment, making complex chronic illness management achievable. To learn how we can support your health goals, visit us at corenurses.com.au.