When people hear the term "aged care nurse," they often picture someone working in a large residential facility. While that's part of the story, the modern role of an Aged Care Registered Nurse (RN) has evolved far beyond that, especially when it comes to in-home care.
So, what exactly is an aged care RN? In short, they are highly skilled clinical professionals who manage the often complex health needs of older Australians and NDIS participants, right in the comfort of their own homes.
Their job is about so much more than basic care. They are the clinical anchor, coordinating with doctors, managing advanced medical treatments, and acting as the central hub for a person's entire healthcare team. This expertise is what allows individuals to live safely and independently, often preventing disruptive and unnecessary trips to the hospital. For instance, an RN can manage a PICC line for intravenous antibiotics at home, saving a client from a lengthy hospital stay for a treatable infection.
Understanding the Modern Aged Care RN Role

Today, the role of an aged care RN is increasingly that of a community-based specialist. This shift is a direct response to what people want: person-centred care that puts their comfort, dignity, and independence first.
It helps to think of an in-home aged care RN as a clinical project manager for your health. They don't just show up to perform tasks; they orchestrate a complete ecosystem of support. They are the critical link that connects you, your family, your GP, and other health professionals, ensuring everyone is on the same page. For example, after a client has a fall, the RN doesn't just treat the injury; they coordinate with a physiotherapist to improve balance and an occupational therapist to make the home safer.
A Leader in Person-Centred Care
One of the most important things an aged care RN does is develop, implement, and constantly review a personalised care plan. This isn't some generic, tick-a-box document. It’s a dynamic strategy built around an individual’s specific health conditions, personal goals, and lifestyle.
Let’s look at a real-world example. Imagine a client living with diabetes who also has a complex wound that won't heal. A skilled RN does much more than just change the dressing. They will:
- Assess the wound meticulously, watching for any signs of infection and applying advanced wound care treatments. For example, they might use a specialised silver-impregnated dressing to combat bacteria.
- Manage the client's insulin routine, making careful adjustments based on blood glucose levels. If a reading is unexpectedly high, they might call the GP to discuss a temporary insulin adjustment.
- Educate the client and their family on how diet and lifestyle can dramatically improve their health, such as by providing a visual guide to carbohydrate counting.
- Liaise directly with the GP and perhaps a podiatrist to make sure the overall treatment plan is working together seamlessly.
This proactive, hands-on approach is key to managing chronic conditions well and preventing the kinds of complications that often lead to hospitalisation. It puts the individual back in the driver's seat of their own health journey. To see the bigger picture, you can learn more about how RNs coordinate with allied health services for truly holistic support.
The ultimate goal of a modern aged care RN is to build capacity and foster independence. They provide the clinical scaffolding that allows individuals with complex needs to remain safely and comfortably in the one place they want to be: their home.
Meeting a Critical Need in the Community
The demand for qualified in-home nursing specialists is climbing, particularly in regions like Sydney and the Wollondilly Shire. As our population ages and more NDIS participants opt for support at home, the clinical leadership of an aged care RN becomes absolutely essential. They are far more than caregivers—they are client advocates, clinical experts, and a cornerstone of our community health system.
What Does an In-Home Aged Care RN Actually Do?

The role of an in-home aged care RN is a dynamic blend of high-level clinical skill, sharp strategic thinking, and genuine compassion. Forget cookie-cutter routines; no two days are the same because no two clients have the same needs, goals, or life circumstances.
To really get a feel for what they do, let's walk through a typical day with one of our Core Nursing Solutions RNs. You'll see firsthand how they tackle complex health challenges right in the comfort of a client's home.
The day kicks off at 8:00 AM with a visit to Mr. Henderson, an NDIS participant who relies on overnight ventilation support. The RN's first job isn't just to ask, "How are you?"—it's to conduct a thorough clinical evaluation from head to toe.
Morning: High-Acuity Care and Assessment
That morning visit is a critical touchpoint. It’s not about ticking boxes; it's about gathering crucial information that shapes the client's care for the rest of the day, and sometimes, the entire week.
For Mr. Henderson, this means:
- Reviewing Oximetry Data: The RN carefully analyses the data downloaded from his BiPAP machine, looking for any concerning dips in oxygen saturation or other patterns from the night.
- Troubleshooting Alarms: He mentions an alarm went off around 3 AM. The RN investigates, quickly finds it was a minor mask leak, and makes a small adjustment to the fit to prevent it from happening again tonight.
- Conducting a Respiratory Assessment: The nurse listens to his breathing, checks his vital signs, and asks about his energy levels to make sure the ventilation support is doing its job effectively.
This kind of hands-on, expert attention is what keeps small issues from snowballing into major health crises. It’s what keeps clients like Mr. Henderson safe at home and out of the hospital, highlighting the specialised nature of the aged care RN role.
The need for this expertise is only growing. Australia is facing a serious nursing shortage, with a projected deficit of over 100,000 nurses by 2026. This puts immense pressure on aged care, especially as our population ages and chronic diseases become more common. In regions from Sydney to Wollondilly, expert management of conditions needing CPAP/BiPAP support or dysphagia care is more vital than ever.
Mid-Day: Clinical Coordination and Complex Care
After making sure Mr. Henderson is stable and comfortable, the RN heads to her next appointment with Mrs. Chan, who is dealing with a non-healing diabetic foot ulcer. This visit is a perfect example of how complex wound management happens in the community.
The RN assesses the wound, carefully noting its size, depth, and any signs of infection. Today, she’s applying a Vacuum-Assisted Closure (VAC) dressing—a specialised treatment that uses negative pressure to accelerate healing. As she works, she talks Mrs. Chan through how to keep the area clean and what warning signs to look out for.
An aged care RN is the crucial link between a client’s home and their wider medical team. Their detailed observations and clear communication are the backbone of effective, coordinated care.
Once the new dressing is on, the RN calls Mrs. Chan's GP. She gives a concise, professional update on the wound's progress, sends a photo (with consent), and discusses the possibility of tweaking the treatment plan. This collaborative loop means the GP has real-time information to make informed decisions, saving Mrs. Chan a difficult and painful trip to the clinic.
Afternoon: Client Education and Family Support
The day's final visit is with Mr. Davies, who needs a routine tracheostomy tube change. This is a delicate procedure that demands precision and a calm, reassuring presence. The RN performs the change efficiently, cleans the stoma site, and makes sure his airway is clear and secure.
But the job isn't just about the clinical task. A huge part of this visit is focused on educating the family. Mr. Davies’ daughter is his primary carer, and she's feeling anxious about a new subcutaneous injection he needs.
The RN sits down with her and patiently:
- Explains the Medication: She describes what the medication is for and its potential side effects in simple, easy-to-understand terms.
- Demonstrates the Technique: She physically shows the daughter how to safely administer the injection, step by step.
- Supervises a Return Demonstration: The daughter then practises giving a mock injection under the RN's watchful eye, which builds her confidence immeasurably.
Empowering clients and their families is at the heart of this work. By arming them with the right knowledge and skills, an aged care RN helps create a supportive home environment, reduces carer stress, and promotes the client’s own independence. Their day is a constant dance between clinical excellence and human connection, making them essential for successful chronic condition management at home.
Aged Care RN vs. Community NDIS Nurse: What’s the Real Difference?
On the surface, "aged care RN" and "community NDIS nurse" might seem like interchangeable terms. Both roles involve highly skilled nursing care, but that's where the similarities end. In practice, they operate in different worlds, driven by vastly different philosophies, settings, and funding models.
Figuring out these distinctions is key to finding the right support. It really boils down to the purpose of the care. Traditional aged care is often focused on maintaining a person’s health and managing existing conditions within a structured facility. Community NDIS nursing, on the other hand, is all about building a person's skills and independence so they can live the life they choose.
The Setting Changes Everything
The most obvious difference is where the care happens. An aged care RN is typically based in a residential facility, looking after the clinical needs of many residents at once. The care they provide is excellent, but it's naturally shaped by the facility's routines and the need to serve a whole community of people. For example, medication rounds might happen at a set time for everyone, regardless of individual preference.
A community NDIS nurse works in a completely different way. Their workplace is your home. This simple fact completely changes the dynamic. Instead of fitting into a facility's schedule, the care is built around you, your goals, and your life. It’s a one-on-one partnership.
This is a critical point, especially here in Australia. We have an aged care workforce of around 370,000, but experts predict a massive shortfall of over 110,000 workers by 2030. As outlined in research on Australia's aged care workforce challenges, this pressure makes specialised, community-based NDIS nurses who can provide complex support even more essential.
Follow the Money: How Funding Shapes Care
The funding model is the engine that drives the entire approach to care. In a traditional aged care facility, funding is allocated to the provider. The facility then creates a care plan based on its own assessments and processes.
The NDIS flips this model on its head. The funding is allocated directly to you, the participant. You are in the driver's seat, choosing who provides your support and how it's delivered. This control is fundamental to the entire scheme.
The NDIS is designed to empower people with disabilities to participate more fully in social and economic life. A community NDIS nurse’s role goes beyond clinical tasks—it's about building the skills and confidence a person needs to live more independently.
Think of it this way: An aged care RN in a facility might be responsible for administering medication to 20 residents every day. A community NDIS nurse would work with a participant over several weeks to help them learn how to safely manage their own medication using a pill organiser and a reminder app. It's about teaching, not just doing. This focus on building life skills is at the heart of what assistance with daily life under the NDIS is all about.
Aged Care RN vs. Community NDIS Nurse at a Glance
To put it all into perspective, this simple table breaks down the key differences between the two roles.
| Aspect | Aged Care RN (Traditional/Facility) | Community NDIS Nurse (e.g., Core Nursing Solutions) |
|---|---|---|
| Primary Focus | Maintaining the health and stability of residents. | Building the skills and independence of the participant. |
| Care Environment | Residential aged care facility or nursing home. | The participant's own home and local community. |
| Funding Source | Aged Care funding allocated to the provider. | NDIS funding allocated directly to the participant. |
As you can see, while both are Registered Nurses, their focus, environment, and the source of their direction are worlds apart. One operates within a system of care for a group, while the other provides highly personalised support designed to empower an individual.
How to Secure NDIS Funding for RN Services
Figuring out how to get NDIS funding for in-home nursing care can feel like you're trying to crack a code. But it gets a lot simpler once you know how to connect your real-life needs to your NDIS goals. The secret is showing that an aged care RN is "reasonable and necessary" for you to live safely, stay healthy, and be part of your community.
It all starts with painting a clear picture of how specialised nursing support helps you achieve your personal goals. Just saying "I need a nurse" won't cut it. You have to draw a straight line from a specific clinical task to the life you want to lead.
Aligning Nursing Needs with NDIS Goals
The NDIS doesn't fund diagnoses; it funds the supports that help you live with them. This means your request needs to focus on how an RN’s skills break down the barriers your disability puts in your way. Most nursing services slot neatly into the 'Improved Daily Living' or 'Improved Health and Wellbeing' support categories.
A great way to frame this is by directly linking the need for a nurse to a specific goal in your plan.
Here’s a practical example:
Goal: "I want to live independently in my own home by managing my health condition safely and avoiding hospital admissions."
Justification: "To achieve this goal, I require an RN for three hours per week to manage my complex wound. This expert care is essential to prevent infection, which would otherwise lead to hospitalisation and a loss of my independence."
See how that works? It shifts the conversation from just "wound care" to the much bigger outcome of "living independently." It clearly spells out why the support is non-negotiable for achieving your NDIS goals.
The process flow below shows how your funding, care setting, and goals are all connected in supporting your life.
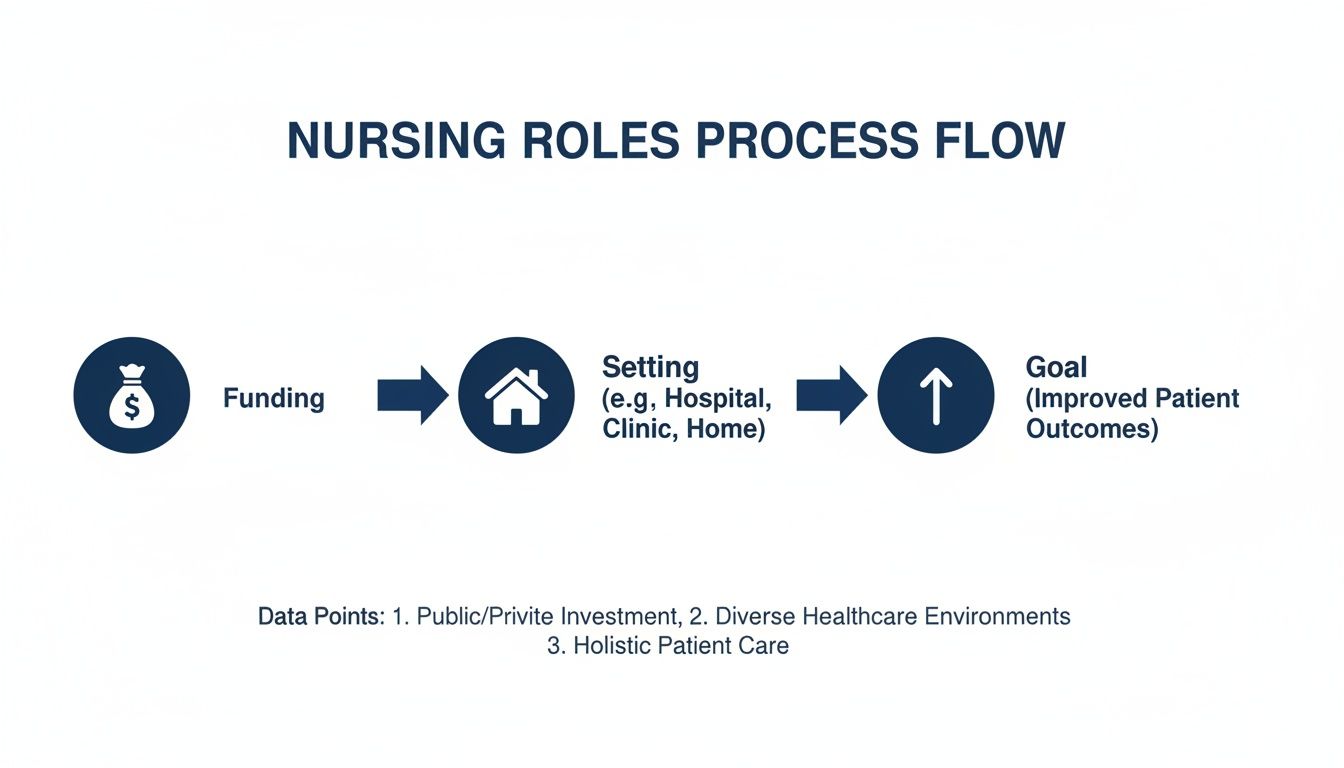
This visual really drives home the point that getting the right funding is the crucial first step to receiving the kind of care that truly helps you hit your goals.
Gathering the Right Evidence for Your Plan Review
Strong evidence is everything when it comes to getting a funding request approved. You'll need solid documentation from qualified professionals that confirms your need for nursing support. Your Support Coordinator can be a massive help in pulling all of this together.
Here’s a checklist of what you should aim to collect:
- A Specialist's Letter: A letter from your GP or specialist is absolutely vital. It should detail your condition and spell out exactly why care from a Registered Nurse is required.
- For instance: "Ms. Smith requires regular tracheostomy care and suctioning from a Registered Nurse to maintain a clear airway. This cannot be safely performed by a support worker and is vital for preventing respiratory complications."
- Functional Capacity Assessment: An assessment from an allied health professional (like an Occupational Therapist) can shine a light on how nursing care helps you with day-to-day functioning and independence. For example, it might state that regular RN care for a catheter reduces urinary tract infections, thereby increasing the client's capacity to participate in community activities.
- Provider Quote and Service Agreement: A detailed quote from a provider like Core Nursing Solutions shows you've done your homework. It outlines the specific services, hours, and costs, which adds a lot of weight to your request. If you need more info on this, you can check out our guide on NDIS service agreements.
Understanding the Billing Process
Once your funding is approved, your provider will deliver the services and claim payment directly from your NDIS plan. This is all done according to the official NDIS Pricing Arrangements and Price Limits, so the process is transparent and regulated. It means you won’t get hit with unexpected out-of-pocket costs for the supports in your plan.
It’s a real shame that while participants desperately need these skilled professionals, many nurses feel their expertise isn't being put to good use. A survey from the Australian Primary Health Care Nurses Association (APNA) found that over half of aged care nurses want to use their advanced skills, but more than a third are held back by employers who don't see a financial reason to let them. This is a big problem in NSW, where nurses make up only 18% of the aged care workforce. You can discover more insights about these workforce challenges from APNA.
Choosing the Right In-Home Nursing Provider in Sydney

Finding the right in-home nursing provider is a massive decision, and it’s about more than just ticking boxes. You’re inviting someone into your home to become a trusted part of your healthcare team—a partner in maintaining your safety, dignity, and independence. Get it right, and it's life-changing. Get it wrong, and you can end up with fragmented care, endless frustration, and poor health outcomes.
In a place like Sydney, the sheer number of options can feel overwhelming. But the key is to look past the glossy brochures and focus on what truly matters: a genuinely person-centred approach. You're not just hiring a nurse; you're choosing a clinical team that takes the time to understand you.
Ultimately, you’re searching for a provider whose aged care RNs have that perfect blend of high-level clinical skill and real, human compassion. That balance is what turns standard care into exceptional support.
Your Essential Checklist for Vetting Providers
When you start talking to potential providers, having the right questions ready is your best defence. It helps you cut through the marketing fluff and get a real sense of their service quality. Think of it as an interview—because you’re hiring them for one of the most important jobs there is.
Use this checklist to guide your conversations and compare different organisations:
- Clinical Specialisation: "Are your nurses specifically trained for my condition? For example, do they have recent, hands-on experience with tracheostomy care or home ventilation support?" General nursing skills simply aren't enough for complex, high-acuity needs.
- Care Coordination: "How exactly do you coordinate with my GP and other allied health professionals?" You're listening for a clear, proactive communication plan, not vague promises. For example, do they use a secure messaging app or provide weekly email summaries?
- Personalised Care Planning: "Walk me through your process for developing and reviewing my care plan. How often is it updated, and how will my family and I be involved?" A good answer will involve regular face-to-face meetings and clear goals.
- Cultural Sensitivity: "How do you make sure your care respects my cultural background, personal values, and end-of-life wishes?" A truly person-centred provider will make this a priority from the very first conversation.
These questions go far beyond simple logistics. They get to the heart of a provider’s commitment to quality, safety, and individualised care—the true hallmarks of a top-tier service.
The Power of Coordinated Care: A Tale of Two Scenarios
To see why this choice is so critical, let’s imagine two different experiences for a man named David, who needs complex wound care and enteral feeding at home.
Scenario 1: The Fragmented Experience
David starts with a provider that has poor coordination. Different nurses show up for different shifts, and none of them seem to know his full story. His care plan feels like a forgotten document. His GP’s office has to constantly chase the provider for updates. A crucial change to his wound dressing gets missed for a week, leading to a minor infection and an avoidable trip to the hospital. David feels like a case file, not a person.
A well-coordinated provider doesn't just manage tasks—they manage outcomes. Their proactive approach prevents complications, reduces hospitalisations, and empowers you to focus on living your life, not just managing your condition.
Scenario 2: The Holistic Approach
Frustrated, David switches to a provider that’s built on coordinated care. He’s assigned a primary aged care RN who becomes his single point of contact. This nurse works with David, his family, and his GP to build a detailed, living care plan.
The RN communicates proactively, sending weekly updates to the doctor and flagging a small issue with the feeding tube long before it becomes a real problem. The result? David’s wound heals faster, he feels more confident and secure at home, and his overall health improves. He feels empowered, and his family feels supported and in the loop. This is the tangible difference a quality provider makes.
To see what this kind of support looks like in practice, you can explore our comprehensive home care services in Sydney.
A Few Common Questions About Aged Care RNs
It's completely normal to have questions when you're looking into clinical support at home. Getting your head around what an aged care RN actually does is the best first step you can take to make a confident choice for yourself or someone you love.
We get asked a lot of the same questions, so we’ve put together some straightforward answers to clear things up. From the nitty-gritty of qualifications to the heart of what they do, here’s what you need to know.
What Kind of Qualifications Does an Aged Care RN Need?
First things first, every aged care RN in Australia must have a Bachelor of Nursing and be currently registered with the Nursing and Midwifery Board of Australia (NMBA). That’s the non-negotiable starting point for any Registered Nurse in the country.
But when it comes to specialised care in your own home, the bar is set much higher. The best providers make sure their RNs don't just stop there; they actively pursue advanced training and certifications for high-acuity skills.
This is what really makes the difference. This extra training is vital for safely managing complex health situations outside of a hospital. Think of things like:
- Advanced techniques for managing chronic or complex wounds.
- Expertise in tracheostomy care, from routine changes to stoma management.
- Competency in handling home ventilation systems like BiPAP and CPAP.
- Specialised training in palliative and end-of-life care.
Having this advanced skillset means the RN brings specific, evidence-based knowledge to the table, ensuring you're not only safe but can also enjoy a better quality of life at home.
Can an Aged Care RN Help With End-of-Life Care at Home?
Yes, absolutely. An experienced aged care RN is a cornerstone of any palliative care team, particularly when someone’s wish is to remain at home. Their role is all about making sure a person’s final chapter is lived with comfort, dignity, and respect.
Their support isn't just about clinical tasks like managing pain and other symptoms. For example, they can set up and manage a subcutaneous syringe driver to deliver continuous pain relief, ensuring a client is always comfortable. They're also there to provide crucial emotional and psychological support for both the individual and their family, helping everyone navigate an incredibly sensitive time with genuine compassion.
An aged care RN's role in palliative care is to honour the individual's wishes. They coordinate with GPs and specialists to create a peaceful and supportive environment, ensuring the person's comfort is the absolute top priority.
This approach is deeply personal and culturally sensitive. It’s about respecting a person's values and beliefs to help create a peaceful experience at home, surrounded by the people who matter most. It’s about fulfilling wishes, not just administering medicine.
How is In-Home RN Care Different From Being in Hospital?
The biggest difference comes down to the environment and the entire purpose of the care. Hospitals are set up for acute medical crises—the focus is on stabilisation. In-home RN care, on the other hand, is all about managing long-term and complex conditions in a place where you feel most comfortable: your own home.
A practical example is diabetes management. In hospital, nurses check blood sugar at set times. At home, an RN works with you to understand how your diet and daily activities affect your levels, teaching you to manage your condition within the rhythm of your own life.
This model is designed to be person-centred, helping to prevent those stressful, disruptive, and often unnecessary trips to the hospital. It also dramatically cuts down the risk of hospital-acquired infections and keeps you connected to your daily routines, family, and community. Put simply, an aged care RN brings hospital-level skills into your world, adapting them to fit your life.
Ultimately, it's a partnership. An in-home RN works with you to build your ability to manage your own health, encouraging independence rather than creating dependence. It’s about empowering you to live the best life you possibly can, right where you belong.
Can I Get RN Support if My NDIS Plan Doesn't Mention It?
You can, and it happens more often than you might think. If your health needs have changed since your last plan, or if they weren't fully understood at the time, you can request a plan review. The trick is to clearly show that RN support is "reasonable and necessary" for you to live safely and work towards your NDIS goals.
To make a strong case, you'll need solid supporting evidence from your GP or a medical specialist. This isn't just a simple letter; it needs to clearly spell out why the specific skills of a Registered Nurse are essential for you to achieve your goals.
Here’s a real-world example of what that evidence could look like:
A letter from a respiratory specialist might say: "Consistent overnight ventilation monitoring and management by a Registered Nurse is required to prevent respiratory distress and avoidable hospital admissions, enabling the participant to remain living safely in their own home."
See how it directly connects the clinical need to the NDIS goal of living independently? A good provider can help you figure out exactly what kind of documentation you need to make the strongest possible case for an aged care RN.
At Core Nursing Solutions Pty Ltd, we know that figuring out complex care can feel overwhelming. Our dedicated team of experienced Registered Nurses is here to provide the expert, compassionate, and person-centred support you need to thrive at home. If you are in the Sydney to Wollondilly region and need specialised in-home nursing care, we are here to help.
Learn more about how our skilled team can support your independence and health goals by visiting us at https://corenurses.com.au.
Pingback: A Guide to Community Health Nursing in Sydney and Wollondilly - Core Nursing Solutions