Living with a long-term health condition like diabetes, heart disease, or arthritis is a journey, not a sprint. Chronic condition management is about putting you in the driver's seat of that journey. It’s a partnership between you and your healthcare team, designed to manage symptoms and improve your quality of life, focusing on staying ahead of problems rather than just reacting to them.
Embracing a New Approach to Chronic Condition Management

Managing a long-term health issue can often feel like a constant juggle. Effective chronic condition management helps shift this from a feeling of uncertainty to one of empowerment. It’s so much more than just taking medication; it’s a structured, collaborative process designed around your life and your goals.
Think of yourself as the captain of your own ship. You know your body, your daily routines, and where you want to go better than anyone. Your in-home nursing team is your skilled crew, helping you navigate the waters, read the maps (your care plan), manage the equipment (your clinical tasks), and coordinate with other experts to ensure your journey is as smooth as possible.
Why Proactive Management Matters
The need for this kind of skilled, in-home support is growing. Across Australia, more and more people are living with long-term health needs. In fact, in 2022, 50% of Australians—that’s around 12.5 million people—were managing at least one chronic health condition. This is a big jump from 42% back in 2007–08, and the number of people with multiple conditions has also risen to 22%. You can find more details on these trends over at Market.us.
These numbers show exactly why a proactive, organised approach is so important. Simply waiting for a crisis to happen can lead to preventable hospital visits and a serious dip in wellbeing. For example, for someone with congestive heart failure, proactive management means a nurse regularly monitors their weight and checks for swelling in their ankles. Spotting a sudden weight gain early allows for a quick call to the GP to adjust medication, preventing fluid buildup that could otherwise lead to a hospital admission.
Effective management isn't about limiting your life; it's about enabling it. By anticipating needs, monitoring symptoms, and coordinating care, we help you maintain your independence and keep doing the things you love, all from the comfort and security of your own home.
The Four Pillars of In-Home Care
A successful strategy for managing a chronic condition at home is built on four key pillars. Each one works together with the others to create a support system that is clinically strong and deeply personal. This framework makes sure that every part of your health is looked after, from daily tasks right through to your long-term goals.
The Four Pillars of In-Home Chronic Condition Management
This table breaks down the core components of our collaborative approach to managing chronic conditions successfully at home.
| Pillar | What It Means for You | Our Role in Your Care |
|---|---|---|
| Personalised Planning | Your care plan is built around your specific health needs, lifestyle, and personal goals, making it practical and truly yours. | We listen to your priorities and collaborate with your GP to design a comprehensive care roadmap that can adapt as your needs change. For example, if your goal is to attend your grandchild's weekly soccer game, we schedule wound care appointments to ensure you're comfortable and ready to go. |
| Clinical Excellence | Complex medical tasks are carried out safely and with compassion in your home, which means fewer stressful trips to a clinic or hospital. | Our registered nurses are skilled in everything from medication administration and wound care to ventilation support. For instance, a nurse can manage a PICC line for IV antibiotics at home, saving you daily trips to a hospital clinic. |
| Team Coordination | Communication between your GP, specialists, and allied health professionals is seamless, ensuring everyone is on the same page. | We act as the central point of contact, coordinating appointments and sharing updates so there are no gaps in your care. An example is relaying a physiotherapist's concerns about mobility to the GP before your next appointment. |
| Empowerment and Education | You and your family gain the confidence and knowledge to understand your condition and take an active part in your own care. | We provide clear explanations, practical training, and continuous support to help you feel in control of your health journey. For instance, we can teach a family member how to recognise the early signs of a urinary tract infection to seek timely treatment. |
By building your support on these four pillars, we ensure your care is not only safe and effective but also empowering, allowing you to live a fuller, more independent life at home.
Creating a Care Plan That Works for You
Your care plan is much more than a clinical document. Think of it as a living roadmap, designed around your life, your goals, and what’s most important to you. Good chronic condition management depends on a plan that is practical and personal. It’s not about fitting you into a pre-made box; it’s about building a support system that fits into your world.
This process always starts with a comprehensive assessment where our main job is to listen. We want to understand your clinical needs, of course, but also your daily routines, hobbies, and personal goals. You are the expert on your own life, and your voice is central to the entire process.
From Listening to Planning
Once we have a clear picture, we start building the plan together. This collaborative approach is essential. It helps us create a strategy that you feel confident in and that genuinely supports your wellbeing.
For example, maybe you need complex wound care but also love your weekly art class. We don’t see those as conflicting priorities. Instead, we’ll build a care schedule that supports both. Your nurse might visit in the morning to handle your wound dressing, making sure you’re comfortable and ready to head out for your class in the afternoon.
This kind of thoughtful scheduling stops clinical needs from getting in the way of the activities that bring you joy. You can find out more about our person-centred approach by reading our guide to chronic illness management services in Sydney.
A great care plan acts like a compass, not a set of rigid rules. It should always point toward your goals for health and quality of life, while being flexible enough to navigate life's detours. It ensures your clinical support enables your life, rather than defining it.
A Dynamic and Collaborative Guide
A truly successful care plan has to be able to adapt. Your health needs can change over time, and your plan must evolve right alongside you. It is never a "set and forget" document.
This means we need to work closely with everyone on your team. We work hand-in-hand with you, your family, your GP, and any other allied health professionals to ensure the plan stays effective.
Here’s how that collaboration works in practice:
- Regular Check-ins: We’ll schedule frequent chats with you to see how the plan is working. For example, after a medication change, we'll check in to ask about side effects and see if the new timing is convenient for your sleep schedule.
- GP and Specialist Updates: Your nurse will keep up clear communication with your doctors. For instance, they might send a weekly summary of your blood pressure readings to your GP, flagging any concerning trends.
- Family and Carer Involvement: With your permission, we involve your loved ones. A practical example is showing a family member how to prepare a meal that aligns with your dietitian's advice for managing diabetes.
This coordinated effort makes sure your chronic condition management strategy is always aligned with your current health and personal preferences. This proactive partnership is the foundation of safe and empowering care at home.
Integrating Clinical Care into Your Daily Life
Managing a chronic or complex condition at home means bringing skilled clinical support right into your personal space. While this can feel like a big step, effective chronic condition management is all about making these necessary tasks feel routine and manageable, so you can live comfortably and confidently. It’s not just about a nurse performing a procedure; it’s about weaving that support seamlessly into the fabric of your day.
Our registered nurses are experts at handling a wide range of clinical duties with both professionalism and genuine compassion. Their goal is to take the stress and uncertainty out of these essential tasks, giving you and your family real peace of mind. By managing these needs at home, we help cut down on those frequent, tiring trips to a clinic or hospital, saving your energy for the things that matter most.
Mastering Day-to-Day Clinical Tasks
Bringing clinical care into your home is a partnership built on trust and expertise. Our team is trained to handle delicate procedures safely and discreetly, making sure your daily life is disrupted as little as possible. We focus on creating a supportive environment where your comfort and dignity always come first.
To do this, we follow a straightforward, collaborative process to develop a care plan that’s built around you.
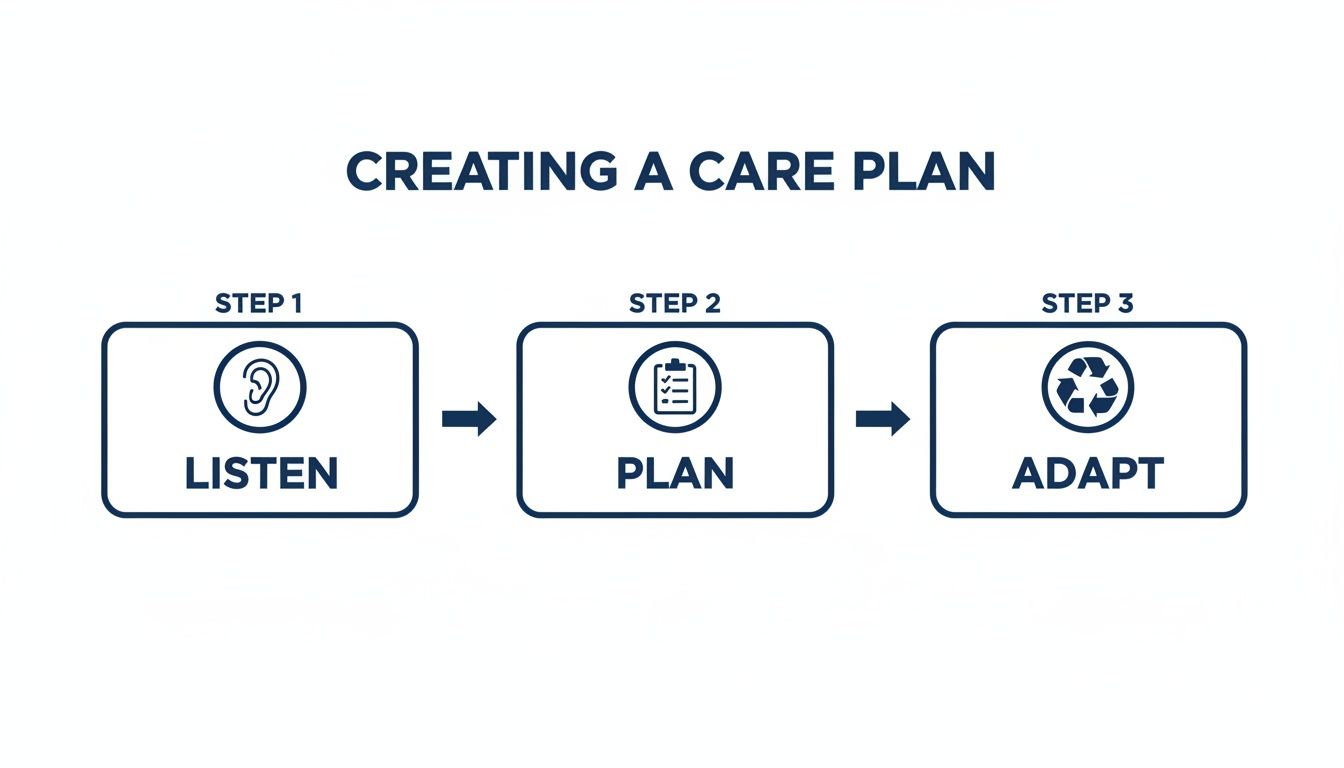
This process ensures every clinical task we perform is part of a plan we've built together. It always starts with your needs and adapts as they change over time.
So, what does this look like in the real world?
Practical Examples of In-Home Nursing Support
Seeing how care works in practice can make it all feel much more approachable. Here are a few common examples of how our nursing team integrates specific clinical tasks into the daily lives of NDIS participants.
Complex Medication Management: Many people need medications that aren’t as simple as taking a pill. For instance, someone with an autoimmune condition might require regular subcutaneous injections. Our nurse can visit at a scheduled time, administer the injection with skill to minimise discomfort, monitor for any side effects, and accurately document everything for your GP. This ensures you get the correct dose on time, every time, without the stress of self-administering.
Overnight Ventilation Support: Living with a respiratory condition like COPD could mean using a BiPAP machine overnight to support your breathing. Our nurse can help set up the equipment, ensure the mask fits perfectly to prevent leaks, and monitor your breathing patterns through the night. This provides a crucial safety net, allowing both you and your family to get a restful, secure night's sleep.
Enteral Feeding Management: For someone unable to eat orally, a Percutaneous Endoscopic Gastrostomy (PEG) tube is a lifeline. Managing it requires strict hygiene and careful monitoring. Our nurse might visit to administer a feed, starting by ensuring the area around the tube is clean and checking for any signs of infection. They then flush the tube, set up the feeding pump with the correct formula and rate, and monitor you during and after the feed to ensure proper digestion. This meticulous process prevents complications and makes sure you receive vital nutrition safely.
Building Confidence Through Compassionate Care
The common thread in all these examples is our focus on making you feel safe and in control. Our nurses don't just perform tasks; they explain what they're doing, answer your questions, and empower you and your family with knowledge. This educational approach is a core part of effective chronic condition management.
For instance, while changing a complex wound dressing, the nurse might explain the signs of healing to look for or show a family member how to spot the early signs of infection. This builds a circle of care around you, where everyone feels more confident and prepared.
The true measure of successful in-home clinical care is not just the perfect execution of a task, but the confidence it inspires. When complex procedures become a predictable part of your routine, it frees you to focus on living your life, not just managing your condition.
This collaborative approach often involves working alongside other specialists, and our nurses are skilled at coordinating with your entire healthcare network. To get a better sense of how these different roles fit together, you can learn more about our allied health services in Sydney. By integrating care with professionalism and compassion, we help turn your home back into a place of healing and independence, not just a clinical setting.
Coordinating Your Entire Healthcare Team

Real success in chronic condition management happens when your whole healthcare team is working together, perfectly in sync. When you're dealing with multiple health needs, it can often feel like you're trying to conduct an orchestra where the musicians have never even met. That’s where your in-home nurse steps in. They become the project manager for your health, making sure everyone is on the same page.
This isn’t just about convenience; it’s about safe and effective care. Your nurse acts as the central hub, connecting you, your GP, your specialists, and any allied health professionals. Because we keep everyone in the loop, we can prevent gaps in care, reduce the stress of managing countless appointments, and ensure your entire team is working towards your goals.
Your Nurse as the Central Hub
Think of your community nurse as the one person who truly understands the complete picture of your health. Because they see how every part of your care plan interacts, they can spot potential issues long before they become serious problems. This central role makes even the most complex care feel manageable.
Let’s imagine someone managing both diabetes and a complex wound. This situation needs input from several experts who might not otherwise talk to each other.
Here’s how a community nurse makes it all work together:
- Endocrinologist: The nurse provides regular updates on blood sugar levels and how the wound is healing. As a result, the specialist can fine-tune the diabetes management plan.
- General Practitioner (GP): Your nurse speaks directly with your GP about any medication changes. This ensures prescriptions are updated and your overall health is monitored.
- Podiatrist: Foot care is absolutely critical for someone with diabetes. The nurse coordinates with the podiatrist to put preventative strategies in place and make sure any foot wound care aligns with best practice.
- Dietitian: Nutrition is key for both blood sugar control and wound healing. Your nurse can share real-world insights with a dietitian to help create a practical meal plan that supports both goals.
This active coordination ensures every professional on your team has the information they need to make the best decisions for you.
Preventing Gaps and Reducing Your Burden
This collaborative style is about more than just clinical efficiency—it's about improving your quality of life. Juggling multiple appointments, repeating your medical history over and over, and chasing up test results is exhausting. When your nurse takes care of this coordination, it lifts a huge weight off your shoulders. A practical example is your nurse arranging for a pathology service to visit you at home for a blood test, then ensuring the results are sent to both your GP and your specialist before your next appointments.
True coordination transforms fragmented care into a unified strategy. It means you spend less time managing the system and more time focusing on your wellbeing, confident that a skilled professional is connecting all the dots behind the scenes.
Australia is known for its high standard of patient care. A landmark OECD survey found we perform well in quality of care (94%), person-centred care (93%), and coordination (74%). But the same report shows that people with multiple conditions often face worse outcomes. Strong coordination is how we close that gap, ensuring even the most complex health needs are managed effectively. You can learn more about these findings on patient experiences with chronic conditions.
By being the central coordinator, we also make sure your NDIS plan and its documentation are clear and well-supported. Our communication creates a solid framework for your care, which is vital for plan reviews and ensuring agreements are properly documented. You can find more information in our helpful guide on creating an NDIS service agreement template. Ultimately, this integrated team effort leads to better health outcomes and a more empowered, confident journey in your chronic condition management.
Using Your NDIS Funding for Nursing Support
Getting your head around how NDIS funding works for clinical nursing care is a huge step in managing a chronic condition at home. It can seem confusing at first, but your NDIS plan is built to be flexible. It’s designed to support the services you need to live safely and on your own terms, and this often includes funding for skilled nurses to handle complex health needs.
Many participants don’t realise their plan can cover these essential clinical tasks. When support is directly tied to a permanent disability—like managing a tracheostomy or monitoring overnight ventilation—it often falls outside the traditional healthcare system. The NDIS is there to fill that gap, making sure you get the continuous, specialised support you need.
Aligning NDIS Supports with Your Clinical Needs
When you look at your NDIS funding, it helps to connect your clinical needs to the specific support categories in your plan. The tasks that help you manage your disability at home often fit neatly into these key areas.
Here are a couple of practical examples:
- Improved Daily Living: This category can fund training for you or your carers. For instance, a nurse could be funded to teach you and your family how to manage your catheter care independently, increasing your self-management skills. It can also cover therapeutic supports, where a nurse assesses your situation and develops a plan to manage your health needs at home.
- Improved Health and Wellbeing: This is often used for services that help you manage the day-to-day impacts of your disability. A practical example would be funding a nurse to provide regular subcutaneous injections or manage complex wound care, which directly prevents hospitalisations and improves your overall health.
The main thing is to show how nursing support helps you chase your goals, build your independence, or get more involved in your community. For example, regular continence care from a skilled nurse might give you the confidence to join social activities. This directly links the support to your goal of community participation. Our guide to NDIS assistance with daily life activities offers more ideas on how these supports fit together.
Preparing for Your NDIS Plan Review
Your plan review meeting is your best chance to make the case for the support you need. Being well-prepared with clear evidence is the key to making sure your funding lines up with your needs for chronic condition management. A detailed report from your nursing provider is one of the most powerful tools you can bring to the table.
Think of your plan review as telling a story backed by facts. The narrative is your life and goals, while the evidence—like nursing assessments and progress reports—provides the crucial details that justify the support you're requesting.
Before your meeting, it’s a good idea to gather all the relevant paperwork. This helps you build a strong case for why ongoing clinical support is "reasonable and necessary" for you.
Your Plan Review Evidence Checklist:
- Comprehensive Nursing Assessment: This is an initial report from a registered nurse that breaks down your clinical needs, the specific tasks involved (e.g., "requires PEG tube management 3 times daily"), and the risks if you don't have skilled support.
- Progress Reports: These are regular updates from your nursing team. A good report might state, "With consistent in-home wound care, the participant's pressure sore has reduced in size by 50% over three months, preventing hospital admission for infection."
- Letters from Your GP or Specialists: A letter from your doctors that confirms your diagnosis and recommends specific in-home nursing care (e.g., "I recommend 10 hours per week of RN support for seizure management") is a vital part of your management plan.
- Your Personal Statement: This is your chance to clearly describe your goals. For example: "My goal is to continue living at home with my family. To do this safely, I need a nurse to manage my ventilator overnight."
Getting this all together helps demystify the process. It turns what could be a stressful meeting into a real opportunity to secure the right level of care for your future.
How We Deliver Person-Centred Care
Properly managing a chronic condition at home is all about trust and expertise. But more than that, it requires a genuine commitment to understanding you as a whole person, not just a set of clinical tasks. At Core Nursing Solutions, we move beyond the checklist. We deliver person-centred care that’s built on evidence, respect, and a clear focus on your goals.
What makes our approach different is our team. Our care is delivered by highly skilled Registered Nurses who have deep experience supporting NDIS participants across Sydney and the Wollondilly region. Because we’re local, we understand the community and are absolutely committed to upholding the highest standards of quality in every home we visit.
Expertise in Complex Care Scenarios
Managing complex health needs at home takes specialised skills and a proactive mindset. Our nurses bring a wealth of experience to even the most high-stakes situations, ensuring your safety and wellbeing are always looked after.
We have proven expertise in managing intricate conditions where precision and constant monitoring are everything. This includes:
- Advanced Tracheostomy Care: Our team is proficient in every aspect of tracheostomy management. This means we handle everything from routine suctioning and dressing changes to emergency response, ensuring you can breathe safely and comfortably.
- Proactive Seizure Management: Working alongside your neurologist, we develop individual seizure plans. Our staff are trained to recognise triggers, administer emergency medication like Midazolam, and provide supportive post-seizure care to ensure a safe recovery.
In everything we do, our approach is built on clear and proactive communication. We make sure you, your family, and your whole healthcare team are kept in the loop. This creates a coordinated circle of support you can truly rely on.
Person-centred care means we see beyond the diagnosis to the individual. We ask, "What does a good day look like for you?" and then build our clinical support around helping you achieve more of those days.
Your Partners in Health and Wellbeing
Ultimately, our goal is to empower you to live the life you choose. We blend clinical excellence with compassionate support to help you achieve your health and lifestyle goals, all within the comfort and familiarity of your own home. Our commitment to quality, safety, and respect is at the heart of our work.
If you’re looking for a partner who can provide skilled, reliable, and truly person-centred chronic condition management, we invite you to have a chat with our team. Let’s discuss how we can support you on your journey.
Frequently Asked Questions About In-Home Care
Figuring out in-home support for chronic condition management can bring up a lot of questions. We’ve put together answers to some of the common queries we get from NDIS participants and their families.
Our goal is to make the whole process clear and simple, so you feel informed and confident every step of the way.
How Do You Ensure Complex Care Is Safe at Home?
Safety is always our highest priority, and it starts with a thorough risk assessment for every person we support. For example, if a client requires overnight ventilation, we assess the home's power supply and ensure a backup power source is available and tested regularly. This lets us see any potential challenges and plan for them ahead of time.
All our staff get ongoing, specialised training for complex clinical tasks, making sure their skills are sharp and up-to-date. We also have clear protocols for escalating any concerns, so there’s a solid plan for every possibility. Most importantly, we keep an open line of communication with your GP and specialists to make sure everyone is on the same page.
Can My Family Be Involved in My Care Planning?
Absolutely. We believe collaboration is key to successful chronic condition management. Your family and loved ones are a huge part of your support network, and we actively encourage their input when we create your care plan.
Collaboration transforms care from a service we provide for you into a partnership we build with you and your family. Involving your loved ones ensures everyone feels confident, supported, and aligned with your health goals.
For example, we can give practical training to family members where it’s appropriate. This might mean teaching a loved one how to spot the early signs of a complication or helping them get comfortable with a piece of equipment, such as a blood glucose monitor. This way, everyone feels included and part of the journey. For those exploring different support options, it can also be useful to understand programs like the Commonwealth Home Support Program.
Which Areas in Sydney Do You Service?
We’re proud to provide our expert in-home nursing and complex care across the greater Sydney metropolitan area and the Wollondilly region. Because we’re local, we understand the communities we work in and have strong connections with local healthcare providers.
Since our service areas are specific, we always suggest getting in touch to confirm we can support you at your exact address. A quick call to our friendly team will give you a clear answer and get the conversation started about your needs.
Ready to talk about how skilled in-home care can support you or your loved one? The team at Core Nursing Solutions Pty Ltd is here to create a personalised plan that helps you achieve your health and lifestyle goals. Contact us today to start the conversation.
Pingback: Living Independently with a Disability: A Practical Guide for Sydney Residents - Core Nursing Solutions
Pingback: Palliative Care Home Care A Guide to Compassionate In-Home Support - Core Nursing Solutions
Pingback: Home Health Care: A Supportive and Person‑Centred for Better Well‑Being - Core Nursing Solutions
Pingback: The Essential Guide to the Aged Care RN Role in Australia - Core Nursing Solutions
Pingback: A Guide to At Home Palliative care in Sydney - Core Nursing Solutions
Pingback: Finding the Right Home Health Care in Sydney - Core Nursing Solutions