When a serious illness enters your life, the focus often shifts entirely to treatments and hospital visits. But what about the person living through it all? That’s where palliative care at home comes in. It is in-home medical support designed to bring comfort and dignity into the picture.
Palliative care in the home isn’t just about managing an illness. It’s about improving your quality of life and easing symptoms and stress. Meanwhile working hand-in-hand with any other treatments you might be receiving. For example, a person undergoing chemotherapy can receive palliative care at home to manage nausea and fatigue. Ultimately this helps them stay strong enough to continue their cancer treatment. It’s about ensuring you or your loved one can maintain a sense of independence and peace in familiar surroundings.
What Palliative Care at Home Really Means

Let’s clear up a common misconception right away. When people hear “palliative care,” their minds often jump straight to the very end of life. But that’s not the whole story. Palliative care is a person-first philosophy of care that can, and should, begin at any stage of a serious illness. It can be provided right alongside curative treatments.
Think of it this way, your doctors are focused on treating the underlying illness. While palliative care at home builds a support system around you and your family. This system is designed to manage pain, relieve difficult symptoms like nausea or breathlessness, and address the emotional and psychological toll. A practical example is a person with advanced heart failure who feels constantly breathless. A palliative care nurse can teach them energy conservation techniques and coordinate with their doctor to adjust medications. In this case, making it easier for them to walk to their garden or sit with family. The ultimate goal isn’t just to manage a condition, but to make each day better.
A Focus on Quality of Life and Dignity
Being able to receive this kind of support at home makes a world of difference. It means staying connected to the routines, people, and community that ground you. For example, being able to sit in your favourite place to have your morning coffee, can provide a sense of comfort. This simple act of being in a familiar space preserves a crucial sense of normalcy and control. This can be incredibly powerful for your mental and emotional wellbeing.
At its heart, palliative care is about making sure every single day can be lived as fully and comfortably as possible. It empowers you to make choices that truly reflect your personal values and wishes.
Sadly, there’s a huge gap between where people want to receive care and where they actually do. While 70% of Australians say they’d prefer to pass away at home, only about 15% are able to. Unfortunately, the vast majority end up in hospitals. This difference shows how vital it is to have high-quality, accessible palliative services that can honour a person’s final wishes.
Understanding the Scope of Support
To really get a feel for what palliative care offers, it helps to see how it fits with other services. This isn’t just about end-of-life support; it’s a broad spectrum of assistance that can be beneficial much earlier in an illness. For a deeper dive into the differences, this guide on Hospice vs. Palliative Care: What Families Really Need to Know is a fantastic resource.
Our approach to home health care is built on these principles, integrating holistic support to bring expert, compassionate care right to your doorstep.
Who Can Benefit From Palliative Home Care

There’s a common myth that palliative care is only for older people or those with terminal cancer. The truth is, the circle of care is much, much wider. Palliative care home care is for anyone, of any age, living with a life-limiting illness who wants to improve their quality of life.
This kind of specialised support is all about managing symptoms and providing comfort, no matter the diagnosis. Palliative home care is designed to focus on the person. Not just their condition. Above all, helping them live as fully and comfortably as possible, for as long as possible.
Think of it as an extra layer of support that works in harmony with existing medical treatments. Designed to make day-to-day life more manageable right in the familiar surroundings of home.
A Broad Spectrum of Conditions
So many different people find immense value in palliative home care. This includes anyone with complex and chronic health needs where managing difficult symptoms is the key to holding onto their independence and wellbeing.
The real focus is on tackling the specific challenges that pop up because of a serious illness. This could be anything from managing persistent pain and breathlessness to navigating the fatigue or emotional stress that often comes with a tough diagnosis.
Some of the conditions where palliative care provides truly critical support include:
- Advanced Chronic Illnesses: This covers conditions like late-stage heart disease, chronic obstructive pulmonary disease (COPD), or kidney failure, where easing symptoms can make a world of difference to daily comfort. For instance, a patient with end-stage renal disease might experience severe itching and fatigue. A palliative care team can help manage these symptoms with specific medications and lifestyle adjustments. Thus, improving their comfort between dialysis sessions.
- Progressive Neurological Disorders: People living with motor neurone disease (MND), Parkinson’s, or multiple sclerosis (MS) benefit hugely from specialised nursing that can adapt as their needs evolve over time.
- Complex Cancers: This isn’t just about end-of-life care. Palliative support can help manage the harsh side effects of treatments like chemotherapy. This is to help improve a person’s strength and ability to tolerate ongoing therapies.
- NDIS Participants with Complex Needs: For participants with life-limiting conditions, palliative care is an essential service that directly supports their goals for independence and quality of life.
Palliative care is not about giving up hope; it’s about adding an extra layer of expert support to help you live better with your illness, on your terms.
For example, a person with advanced motor neurone disease might need help with in-home ventilation to manage their breathing. Our specialised nurses can provide this exact care at home, which means fewer trips to the hospital and more time spent in a comfortable, familiar place with family.
Another real-world example is someone with diabetes who has developed chronic, hard-to-heal wounds. Our nurses can deliver advanced wound management at home, which not only reduces pain and the risk of infection but also actively promotes healing.
Navigating Funding and Access
Working out how to fund palliative care home care can feel overwhelming, but it’s a crucial step. In Australia, there are a few different pathways, and helping families navigate them is a core part of what we do. We’re here to help families and support coordinators secure the right care through the best funding stream for their situation.
- NDIS (National Disability Insurance Scheme): For eligible participants, NDIS funding can be used for in-home nursing and support services that fall under the palliative care umbrella, especially when the need is linked to a permanent and significant disability. For example, an NDIS participant with Huntington’s disease could use their funding for a support worker to assist with daily tasks and a nurse to manage swallowing difficulties.
- Medicare: Some services from GPs and specialists who are part of a palliative care plan may be subsidised through Medicare.
- Private Funding: Many families choose to fund services privately. This can supplement other programs or simply offer more direct control over the type and frequency of care received.
Our team will work closely with you, your family, and your support coordinator to explore all these avenues. We provide clear, straightforward advice on eligibility and help design a care plan that fits within your available funding, ensuring you get the compassionate, expert support you need at home.
What Does Palliative Care at Home Actually Involve?
When you hear the term palliative home care, it’s easy to think of ideas like comfort and quality of life. But what does that really mean on a practical, day-to-day basis? It means having a skilled, compassionate team bring a specific set of services right to your door, tackling the real-world challenges of living with a serious illness.
These aren’t just items on a checklist. They’re tangible actions that relieve pain, preserve dignity, and help someone live as fully as possible in the one place they feel most at ease—their own home. Think of each service as a building block, creating a robust support system for both the person needing care and their family.
This support comes from a dedicated team of registered nurses and trained support workers. They bring clinical expertise and genuine empathy together to manage complex medical needs that would otherwise mean a trip to the hospital.
Specialised Nursing for Complex Symptom Management
One of the absolute pillars of palliative care at home is managing difficult symptoms. A serious illness often brings a heavy burden of pain, nausea, constant fatigue, or breathlessness. These symptoms can be completely draining, making even the simplest daily activities feel like climbing a mountain.
Our specialised nurses are experts at assessing and managing these complex issues. It’s about so much more than just giving out medication. It’s about getting to the root cause of the discomfort and creating a proactive plan to stay one step ahead of it. The whole point is to bring relief and stability, so the person can focus on what’s truly important to them.
Take, for example, someone with advanced lung disease who is constantly short of breath. Our nurse would step in to:
- Administer prescribed medications to make breathing easier.
- Teach gentle breathing exercises and ways to conserve energy.
- Help find comfortable positions that optimise lung function.
- Liaise directly with their GP or respiratory specialist to fine-tune the care plan.
This hands-on, forward-thinking approach can turn a frightening symptom into something that can be managed.
Advanced Medical Support in Your Own Home
Many people needing palliative care also have complex medical needs that, until recently, meant being in a hospital. High-quality palliative care home care changes that by bringing this advanced support right to you, avoiding the stress and exhaustion of constant hospital visits.
Being able to receive advanced medical care at home is a game-changer. It shifts the focus away from travel and appointments, and back to simply being present with loved ones in a familiar, comfortable space.
Our skilled nursing team is experienced in a wide range of complex procedures, ensuring care is safe, consistent, and reliable. A practical example is managing a subcutaneous pain pump for a person with cancer, which delivers continuous pain relief without the need for constant injections, all managed by a nurse in the home.
Before we dive into the specifics, this table provides a quick overview of the key services you can expect and why they matter.
Palliative Home Care Services at a Glance
| Service Category | Specific Services Provided | Primary Goal/Benefit |
|---|---|---|
| Symptom Management | Pain relief, nausea control, fatigue & breathlessness support. | To provide physical comfort and stability, allowing for better quality of life. |
| Enteral Feeding | PEG tube management, feed/medication administration, site care. | To ensure safe and adequate nutrition when swallowing is difficult. |
| Respiratory Support | Tracheostomy care, non-invasive ventilation (CPAP/BiPAP) support. | To maintain clear airways and support breathing, especially during rest. |
| Wound & Catheter Care | Complex wound dressings, indwelling & suprapubic catheter management. | To prevent infection, manage pain, and maintain dignity and hygiene. |
| Personal & Daily Care | Assistance with mobility, hygiene, and daily routines. | To preserve independence and dignity in everyday life activities. |
This summary highlights how each service is designed not just to treat a condition, but to enhance the overall well-being of the individual in their home environment.
Key Medical Support Services
- Enteral Feeding Support: For those who can no longer eat or drink safely (dysphagia), we manage Percutaneous Endoscopic Gastrostomy (PEG) tubes. Our nurses don’t just administer feeds; they provide meticulous site care to prevent infection and teach family members how to handle everything safely. For example, a nurse can teach a spouse how to properly flush the tube to prevent blockages, empowering them to participate in care confidently.
- Tracheostomy and Ventilation Care: We offer expert care for clients with tracheostomies, covering routine cleaning, dressing changes, and emergency management. We also support non-invasive ventilation (NIV) like CPAP and BiPAP machines, ensuring the equipment is used correctly to support breathing.
- Complex Medication Management: This can involve anything from administering injections to managing complex pain relief through subcutaneous infusions. We monitor closely for side effects and work hand-in-glove with the prescribing doctor to make sure the medication plan is working as it should.
Personalised Daily and Continence Care
Dignity is at the heart of everything we do. That absolutely extends to the most personal aspects of daily life, like managing wounds or continence. These can be sensitive areas that cause a lot of discomfort and distress if not handled with skill, respect, and discretion.
Our team provides expert care for complex and chronic wounds, using proven dressing techniques to promote healing, manage pain, and prevent infection. This is especially vital for people with limited mobility or conditions like diabetes that slow down the healing process.
Likewise, we offer discreet and effective continence care, including managing catheters (both indwelling and suprapubic). Our nurses ensure everything is working correctly, perform routine changes, and watch for any signs of infection—all while protecting the client’s privacy and comfort. By bringing this level of clinical skill into the home, we work alongside other specialists to provide a complete circle of care. You can learn more about how we coordinate with allied health services to get the best possible outcomes for our clients.
How Coordinated Care Planning Works
Delivering exceptional palliative care at home is never a one-person job. It’s a carefully orchestrated team effort, where high-quality support comes from making sure every piece works together seamlessly. This synchronisation doesn’t happen by accident; it’s the result of detailed, collaborative care planning.
Think of a care plan as the master blueprint for a person’s health and comfort. It’s not some static document we create in an office. Instead, it’s a living, breathing guide that evolves through real conversations between the client, their family, our nursing team, and their trusted doctors, like their GP and other specialists. This way, everyone is on the same page, working towards the same goals.
The whole process kicks off with a person-centred assessment. We take the time to listen, to understand not just the clinical needs but also the individual’s personal values, lifestyle, and what a “good day” truly looks like for them. For example, if a client’s main goal is to be well enough to sit in their garden for an hour each afternoon, the entire care plan—from medication timing to physiotherapy exercises—will be built around making that happen. That understanding becomes the bedrock of a plan that genuinely respects their wishes.
Building a Collaborative Care Team
Once we have that initial plan, the real coordination begins. Our job is to be the central hub, connecting all the different threads of a person’s healthcare journey. This proactive communication is what stops care from becoming fragmented, where different providers might accidentally give conflicting advice.
We stay in regular contact with GPs, specialists, and allied health professionals—from physiotherapists to dietitians. This ensures the support we provide at home is always perfectly aligned with the broader medical strategy. It’s a dynamic process of sharing updates, tweaking plans as needed, and solving problems as a team.
Here’s a practical example: our Registered Nurse might join a case conference with a client’s GP and respiratory specialist. In that meeting, they can align the in-home ventilation support directly with the client’s medical goals, ensuring the hands-on care at home is actively supporting the specialist’s treatment plan. This kind of collaboration is a vital part of effective chronic condition management at home.
This diagram helps show how different services come together under one holistic approach, focusing on symptom control, medical support, and help with daily living.
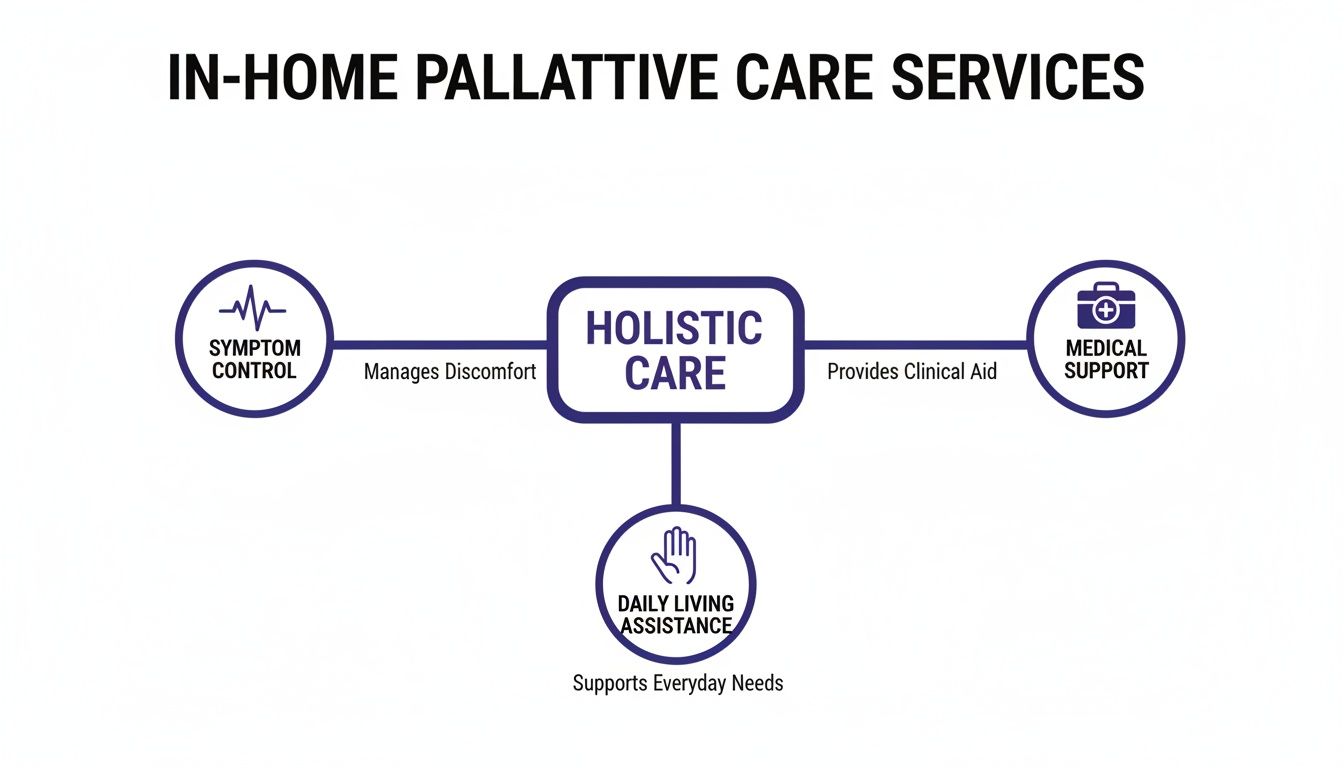
It makes it clear that palliative care is a multi-faceted approach, where medical expertise and personal support are equally important for a person’s overall wellbeing.
The Vital Role of Advance Care Planning
A crucial part of coordinated care involves looking ahead. Advance Care Planning (ACP) is simply the process of thinking about, discussing, and documenting your preferences for future healthcare. It’s about making sure your voice is heard, even if you get to a point where you can no longer speak for yourself.
This isn’t just about end-of-life decisions. It’s about defining your values and what quality of life means to you. An Advance Care Directive is the formal document where these wishes are recorded, allowing you to appoint a trusted person to make decisions on your behalf and outline the types of treatments you would or would not want.
Advance Care Planning is one of the most powerful gifts you can give your family. It removes the burden of guessing your wishes during a stressful time and ensures your care journey unfolds according to your values.
Despite how important it is, there’s a big gap in preparedness. A recent Australian study found that only 33% of adults have done any form of advance care planning. Even more surprisingly, just 12% had talked about their wishes with a healthcare professional, even though they saw them as trusted advisors. You can dig into the full findings on palliative care preparedness in Australia.
Our team champions this process. We guide clients and families through these significant conversations with sensitivity and respect. We help translate personal values into clear directives so the entire care team—from our nurses to hospital staff—can understand and honour their wishes, giving everyone true peace of mind.
Supporting Families and Carers Through the Journey

Palliative care isn’t just about the person who is unwell. It’s a circle of support that wraps around the family and carers who are right there with them, every step of the way. Loved ones often take on an incredible amount of responsibility, from managing complex medications to simply being a source of comfort. It’s a role that can be profoundly rewarding, but also immensely challenging.
Truly great palliative care home care understands this reality and actively supports the entire family. By easing the pressure on primary carers, we help prevent exhaustion and ensure the best possible care is consistently delivered. It’s all about creating a sustainable, positive, and supportive environment for everyone.
We don’t see families as bystanders; we see them as vital partners. This approach builds a foundation of trust, open communication, and a shared commitment to what matters most.
Practical Support to Ease the Burden
The day-to-day challenges for families are both practical and emotional. Our services are designed to offer real, tangible relief and expert guidance exactly when it’s needed. We’re not here to take over, but to reinforce the family’s efforts with professional skills and the chance for a much-needed break.
Here’s how we can help:
- Skills Training: We can show family members safe and effective techniques for daily tasks, like helping someone move from a bed to a chair or assisting with personal care. For example, a nurse can demonstrate the correct way to use a hoist, which builds a carer’s confidence and helps keep everyone safe from injury.
- Clear Communication: Our team makes a point of providing regular updates and clear, simple explanations about the care plan. This helps reduce the uncertainty and anxiety that naturally comes with managing a serious illness at home.
- Respite Care: This is often the most crucial support we offer. For instance, respite gives primary carers a chance to step away, rest, and recharge, knowing their loved one is in safe, professional hands.
A family-inclusive approach ensures that carers are not just supported, but are also empowered as valued members of the care team, whose insights are crucial to delivering truly person-centred care.
It is so important for carers to recognize the signs of emotional burnout to protect their own health. Having professional backup is one of the best ways to prevent this from happening.
Real-World Examples of Family Support
Let’s look at a common scenario to see how this works in practice. Imagine a wife caring for her husband, who needs to be monitored overnight because of breathing difficulties. She’s exhausted from lack of sleep and constant worry, which is starting to affect her ability to look after him during the day.
This is where one of our trained support workers can provide overnight supervision. This simple but vital service means his wife can get a full night’s sleep, giving her total peace of mind that a professional is there to handle anything that comes up.
Here’s another example: a son is caring for his mother and finds it difficult to help her with personal hygiene tasks. Our team can provide sensitive and dignified help with these daily routines, which you can read more about in our guide to assistance with daily life. This support helps preserve their family relationship, allowing the son to focus on being a loving son, rather than performing tasks that can sometimes feel awkward for everyone.
This is how professional palliative care home care works to strengthen family bonds during one of life’s most difficult times.
How to Arrange Palliative Care in Sydney
Organising specialised palliative care home care for someone you love can feel overwhelming, but it doesn’t have to be. For families, support coordinators, and hospital discharge planners across Sydney and Wollondilly, the whole process is designed to be as clear and supportive as possible. It all begins with a simple conversation.
Our goal is to get a robust support system in place quickly, easing the stress on everyone and putting comfort first. It starts with a confidential chat so we can understand your unique situation and what you need most right now.
Your First Step: The Initial Phone Call
Making that first call is the most crucial step. Whether you’re a family member looking for answers, an NDIS support coordinator arranging services, or a hospital discharge planner ensuring a safe transition home, our team is here to listen.
During this call, we’ll gently guide you through a few questions to get a clear picture. It helps if you have some information handy, but please don’t worry if you don’t have all the answers. That’s what we’re here for – to help you figure it all out.
This first conversation isn’t just about logistics. Moreso, it’s about starting a relationship built on trust and understanding from the very beginning. We want to hear your story so we can figure out the best way to help.
Preparing for Your Conversation
To help us create the most effective care plan, having a few key details on hand can make a real difference. This information gives us a clearer view of both the clinical needs and personal preferences, ensuring the care we provide is a perfect fit.
If you can, try to have this information ready:
- A brief medical history: Just the main diagnosis and any other important health conditions. For example, “Dad has COPD and also Type 2 diabetes.”
- Current care needs: What are the biggest challenges at the moment? This could be anything from managing pain to needing help with mobility or medications. For example, “Mum is having trouble getting out of bed and needs help with her wound dressings.”
- Contact details for the GP or specialists: This allows us to start coordinating with their existing medical team straight away.
- Funding information: If you know it, details about an NDIS plan, private health insurance, or other funding sources are helpful.
From Assessment to Action Plan
After that initial call, the next step is a comprehensive in-home assessment. One of our Registered Nurses will visit to meet the client and their family in person. This gives us a chance to see the home environment and have a proper chat about needs and goals.
Based on that assessment, we create a person-centred care plan. This isn’t just a document; it’s a clear, practical roadmap that outlines exactly what services will be provided, when they’ll happen, and who will be there. It ensures that everyone involved—from our nurses to your GP—is working together seamlessly to provide compassionate and effective palliative care home care.
To learn more about the different types of support available, explore our detailed guide on home care services in Sydney.
Your Palliative Home Care Questions Answered
When you’re exploring palliative care, it’s natural to have a lot of questions. Getting clear, straightforward answers is the first step to feeling in control and making the best decisions for your family. We’ve gathered some of the most common questions we hear to help clear things up.
Our goal here is to cut through the confusion and give you practical information, so you can move forward with confidence.
Is Palliative Care Only for the Last Few Days of Life?
Absolutely not. This is probably the biggest and most persistent myth out there. The truth is, palliative care is most effective when it starts right at the time of diagnosis of a serious illness. Furthermore, it can run alongside curative treatments for months, or even years.
The whole point is to improve quality of life by getting on top of symptoms and stress, no matter what stage you’re at. For example, someone going through chemotherapy can use palliative care to manage the tough side effects like nausea and fatigue. This often helps them stay strong enough to continue with their cancer treatment.
Can I Keep My Own Doctor and Specialists?
Yes, of course. In fact, we insist on it. Palliative care is designed to work with your existing medical team, not replace them. To illustrate, think of our nurses as an extra, specialised layer of support who communicate and coordinate with your GP, oncologist, or other specialists.
Our palliative care team becomes a crucial communication bridge. We make sure the care you receive at home aligns perfectly with your doctor’s overall treatment plan and goals.
For instance, our Registered Nurse might speak directly with your GP about how a new pain medication is working, allowing for quick adjustments without a trip to the clinic. This teamwork ensures your care is seamless, consistent, and always focused on you.
How Is Palliative Home Care Funded?
In Australia, funding for palliative care home care can come from a few different places, and our team is experienced in helping families figure out the best path. The main options are:
- NDIS (National Disability Insurance Scheme): If you or your loved one is an NDIS participant with a permanent and significant disability, your funding can often be used for in-home nursing and other palliative support services.
- Private Funding: Many families choose to pay privately. This gives you the most flexibility and direct control over the type and frequency of care you receive.
- Medicare and Private Health Insurance: Medicare will cover your GP and specialist appointments. However, it generally doesn’t cover the cost of private nurses in your home. Some top-tier private health insurance policies might offer rebates, so it’s always worth checking your policy details.
Unfortunately, the healthcare system can sometimes struggle to connect people with the support they need. In 2021-22, only 4,800 people in residential aged care were officially identified as needing palliative care, a tiny fraction of the 245,000 who moved into care that year. This shows a massive gap that quality home-based care can help fill, as highlighted in this report on palliative care resourcing for older Australians.
We can sit down with you, look at your specific circumstances, and help you find the most suitable funding stream. We want to make sure you get all the support you’re entitled to.
Ready to talk about how specialised, compassionate care at home could make a difference? The team at Core Nursing Solutions Pty Ltd is here to listen and provide clear, expert guidance.
Contact us today for a confidential discussion about your needs.