Allied health services are specialised therapies delivered by university-trained health experts who aren't doctors or nurses. Their main purpose is to help you manage daily life, grow your independence, and hit your personal goals. These services are often the cornerstone of a successful NDIS plan, offering targeted support to build your skills and abilities. For instance, a physiotherapist might create an exercise plan to improve your balance, while an occupational therapist could help you adapt your kitchen to make cooking easier.
What Allied Health Services Mean for Your NDIS Plan

Think of your NDIS journey as pulling together a dream team for a very special project—your success. Allied health services are the core experts on that team. These are highly skilled professionals who provide specialised care and therapies to help you live more safely and independently.
Let's use an analogy to make it simpler. Imagine your NDIS plan is the blueprint for a custom-built home, designed just for you. Your allied health professionals are the master craftspeople who bring that blueprint to life, each with a very specific role.
The Craftspeople Building Your Independence
In this picture, different specialists contribute their unique skills to the project. The final structure and function of your home depend on their coordinated expertise. For example:
- An Occupational Therapist acts like the interior designer, figuring out how to redesign the kitchen so it’s fully accessible for a wheelchair user. A practicable example would be installing a height-adjustable countertop or suggesting long-handled cooking utensils.
- A Physiotherapist is the structural engineer, making sure hallways and doorways are safe to navigate and strengthening the foundations to prevent falls. For example, they might prescribe specific leg-strengthening exercises or recommend installing grab rails in the bathroom.
- A Speech Pathologist works as the communications expert, wiring up systems that make it easier for you to express your needs and connect with family and friends. A real-world example is programming a communication device with phrases for ordering coffee or talking about a favourite hobby.
Each professional focuses on a different part of the build, but they all work towards the same goal: creating a perfectly functional and supportive home for you.
These professionals aren't just consultants; they provide hands-on, evidence-based therapies to develop your skills, improve how you function, and boost your overall wellbeing. Their work is central to achieving the goals laid out in your NDIS plan.
Connecting the Blueprint to Daily Life
So, where do our in-home nurses fit into all this? Think of our nursing team as the on-site project manager. They make sure the expert plans from your allied health team are followed correctly, every single day.
Our nurses are the ones on the ground, integrating the physiotherapist’s exercises into your daily routine or ensuring the mealtime plan from a dietitian is implemented safely. This proactive management is a key part of our approach to chronic illness management, and it ensures expert advice translates into real-world progress. For example, if a dietitian recommends a low-sodium diet, our nurse can assist with meal preparation and monitoring blood pressure, providing direct feedback to the dietitian.
By working directly with these specialists, our in-home nurses bridge the gap between a therapy session and your everyday life. They bring expert, coordinated care right into your home, making sure the blueprint for your independence becomes a reality. This close collaboration is vital for making your NDIS plan a practical success.
Meet Your Potential Allied Health Team

Trying to figure out which allied health services you need can feel like reading a map without a legend. So many professional titles sound alike, but their roles are actually quite distinct and specialised.
The best way forward is to move past the jargon and focus on the practical, life-changing support they really offer. Each professional brings a unique set of skills to the table, all designed to help you build your capacity, boost your independence, and hit your specific NDIS goals.
Let's meet some of the key players you are likely to encounter on your journey.
Occupational Therapists: The Architects of Daily Living
An Occupational Therapist (OT) is all about your "occupations"—which are just the meaningful activities that fill up your day. This isn't just about your job. It includes everything from showering and cooking to enjoying hobbies and getting out into your community.
Put simply, an OT looks at the challenges you face in daily tasks and finds practical ways to solve them. They are the problem-solvers who help you adapt your environment or learn new techniques to get things done.
Practical Example: A young adult with autism wants to find a job but finds morning routines and organisation a real challenge. An OT could work with them to create a visual schedule for getting ready, practise the bus route to work, and come up with strategies for managing sensory overload in a busy office. It’s all about building the skills and confidence they need to succeed at work.
Physiotherapists: The Movement and Mobility Experts
A Physiotherapist, or physio, is an expert in how the human body moves. Their focus is on improving your physical function, strength, balance, and mobility, helping you move more freely and with less pain. Their goal is to maximise your physical potential and lower your risk of injury.
To do this, they use a whole range of techniques. This can include tailored exercise programs, massage, and recommending the right mobility aids to help you stay active and safe.
Practical Example: An older person who has had a few falls is starting to feel afraid of leaving their home. A physio would assess their strength and balance, then design a home exercise program to build up their leg and core muscles. They might also suggest safer ways to use the stairs and recommend a specific walking aid, helping them get their confidence back so they can reconnect with their community.
Speech Pathologists: The Communication Champions
A Speech Pathologist, often called a "speechie," supports every aspect of communication. This covers speaking, listening, understanding language, reading, writing, and using social skills. They also play a critical role in assessing and managing swallowing difficulties, known as dysphagia.
Ultimately, their work empowers people to express themselves, connect with others, and take part more fully in life.
Practical Example: Someone who has had a stroke is having trouble finding the right words and can't swallow certain foods safely. A speech pathologist would provide therapy to rebuild their language skills. At the same time, they would create a texture-modified diet plan with safe swallowing strategies. This makes sure mealtimes are both enjoyable and safe while helping them communicate their needs to family and carers.
The real value of allied health services is their focus on practical outcomes. It’s not just about the therapy itself, but about how that therapy translates into tangible improvements in your everyday life and helps you achieve your NDIS goals.
Dietitians: The Nutrition and Wellbeing Guides
A Dietitian gives expert advice on food and nutrition to improve your health and manage medical conditions. They use evidence-based science to create personalised eating plans that meet your specific health needs and personal preferences.
They are different from nutritionists because dietitians are qualified to provide medical nutrition therapy for complex conditions. This is a key part of our person-centred disability home care services, where we integrate nutrition into the overall care plan.
Practical Example: An individual has just been diagnosed with Type 2 diabetes and coeliac disease and feels completely overwhelmed. A dietitian would develop a meal plan that is both gluten-free and manages their blood sugar levels. They would also teach them how to read food labels, offer simple recipes, and help them build a healthy and enjoyable relationship with food again.
To help you see how these roles connect to your plan, here’s a quick breakdown of how common allied health professionals can support your NDIS goals.
How Common Allied Health Professionals Support Your NDIS Goals
| Allied Health Profession | Practical Examples of Support | Relevant NDIS Support Category |
|---|---|---|
| Occupational Therapist | Prescribing assistive technology (like a specialised chair), teaching new ways to cook, creating sensory plans, and adapting your home for better access. | Improved Daily Living |
| Physiotherapist | Creating an exercise program to build strength, improving balance to prevent falls, managing pain, and recommending mobility aids like walkers. | Improved Daily Living, Health and Wellbeing |
| Speech Pathologist | Helping with speech clarity, using communication devices, managing safe swallowing, and building social interaction skills. | Improved Daily Living, Improved Relationships |
| Dietitian | Creating meal plans for medical needs (like diabetes), advising on tube feeding, managing food allergies, and promoting healthy eating habits. | Improved Daily Living, Health and Wellbeing |
| Psychologist | Providing therapy for mental health, developing behaviour support plans, and helping with emotional regulation and coping strategies. | Improved Daily Living, Improved Relationships |
| Podiatrist | Managing foot care for high-risk individuals (e.g., with diabetes), prescribing custom orthotics, and treating foot and lower limb pain. | Improved Daily Living, Health and Wellbeing |
These are just a few of the many professionals who might join your team. Your specific needs and goals will always determine which allied health services are right for you.
How In-Home Nursing and Allied Health Work Together
True success in complex care isn't just about individual experts; it comes from seamless, coordinated teamwork. While your allied health specialists provide the expert strategies for building skills, it's the in-home nurses who turn those strategies into daily progress. This powerful synergy is what truly helps you achieve your goals.
Think of it like a symphony orchestra getting ready for a big performance. Your GP is the conductor, setting the overall direction and pace. The allied health team—your physio, OT, speech pathologist—are the different instrument sections, each contributing their unique expertise.
In this picture, our in-home nurses are the lead musicians on the ground. They're there every day, making sure the conductor's vision is realised and that every section plays in perfect harmony. They don't just focus on their own part; they listen to everyone else, making sure the whole piece flows beautifully.
Turning Therapy Plans into Daily Habits
An allied health professional might visit for an hour once a week, but your health is a 24/7 reality. This is where the partnership with in-home nursing becomes so crucial. A nurse in your home provides the consistent, day-to-day reinforcement needed to make therapeutic strategies stick.
This continuous support bridges the gap between appointments. As a result, expert advice is transformed into ingrained daily habits and skills that last.
The real goal is to move beyond isolated therapy sessions. We aim to create a supportive environment where therapeutic activities are woven into the fabric of your everyday life, making progress feel natural and sustainable.
For example, a physiotherapist might create an exercise plan to improve your strength and reduce your risk of falls. Our in-home nurses don't just supervise these exercises—they are trained to do much more, creating a vital feedback loop.
- Integration: They find clever ways to fit exercises into your daily routine, like doing balance practice while you wait for the kettle to boil.
- Monitoring: They watch closely for any signs of pain, fatigue, or difficulty, knowing exactly when to encourage you and when to ease back.
- Feedback: They provide real-time, detailed feedback directly to the physiotherapist, so your plan can be adjusted quickly for better results.
This collaborative approach means that therapy plans aren't just attempted; they're consistently and safely applied. This leads to faster progress, safer management of complex conditions, and a big reduction in preventable hospital visits.
A Practical Example of Teamwork in Action
Let's look at a real-world scenario to see how this all comes together.
The Client: An NDIS participant named David has dysphagia (difficulty swallowing) after a hospital stay and is at high risk of choking. He also has complex medication needs.
The Allied Health Team:
- A Speech Pathologist assesses David. They create a texture-modified diet plan (minced and moist foods) and teach him specific safe swallowing techniques.
- A Dietitian develops a nutritionally complete meal plan that works within the speech pathologist's texture requirements.
The In-Home Nursing Role:
Our registered nurse becomes the central point of action. They don't just follow the plan; they actively manage it.
- Mealtime Support: The nurse ensures every single meal is prepared to the exact texture specifications. They personally assist David, cueing him to use the safe swallowing techniques from the speech pathologist.
- Medication Management: They crush specific medications and mix them with the right food consistency. This ensures David gets his essential medicine safely without putting his swallowing plan at risk.
- Observation and Reporting: The nurse meticulously documents how David tolerates each meal, noting any signs of coughing or distress, and tracking his hydration and nutrition. This detailed data is then shared with both the speech pathologist and dietitian.
Because of this constant oversight, the speech pathologist can confidently fine-tune David's plan based on the nurse's detailed reports. As a result, David can progress to less modified food textures more quickly and safely. You can learn more about how we implement such detailed plans in our guide to home care services in Sydney.
This integrated system ensures the expert recommendations from allied health services are implemented flawlessly. In short, it protects David’s health while actively helping him regain his skills.
How to Fund Allied Health Services Through Your NDIS Plan
Understanding how to get the right funding is a huge part of making your NDIS plan work for you. The process can seem a little complicated at first, but once you know what’s needed, you can confidently ask for the resources to help you reach your goals.
Funding for allied health isn’t just about paying for appointments. It’s an investment in your independence and ability to build new skills. The NDIS is designed to support this kind of growth, but it all comes down to showing a clear link between the therapy you need and the outcomes you want to achieve.
Understanding Your Capacity Building Budget
Most allied health services fall under the Capacity Building support category in an NDIS plan. Think of this budget as your personal development toolkit. It’s set aside specifically for supports that help you build your skills, become more independent, and get more involved in your community.
This funding is about much more than just attending therapy sessions. It’s an investment in learning new ways to manage daily life, improve your mobility, or communicate more effectively. So, when you ask for funding for an OT or a physio, you're really asking for the tools to become more self-sufficient. For example, funding a psychologist isn't just for therapy sessions; it's for learning coping strategies to manage anxiety when you go grocery shopping, which directly builds your capacity for community participation.
To get this funding approved, you have to clearly connect the dots for the National Disability Insurance Agency (NDIA). They need to see exactly how these services will help you work towards the specific goals written in your plan.
Preparing for Your NDIS Planning Meeting
Your planning meeting is the perfect time to make a strong case for the funding you need. The key is to be prepared. Instead of speaking in general terms, you’ll want to use concrete examples that tie directly back to your goals.
The best way to approach it is to frame your needs as actions toward a goal. This turns a vague wish into a clear, measurable plan and gives the NDIA a solid reason to approve the funds.
For example, simply saying "I want to be healthier" doesn't give the planner much to work with. But if you can explain how you plan to get there, it paints a much clearer picture of the support you need.
Practical Examples of Goal Framing:
Vague Statement: "I want to be more mobile."
Goal-Oriented Request: "To improve my mobility so I can safely access my community, my physiotherapist recommends 20 hours of therapy. This will help me build strength and balance, which will reduce my risk of falls."
Vague Statement: "I need help with my communication."
Goal-Oriented Request: "To achieve my goal of joining a local book club, I need 30 hours of speech pathology. This will help me work on my conversational skills and build confidence in social settings."
This simple process of planning, taking action, and getting feedback is powerful.
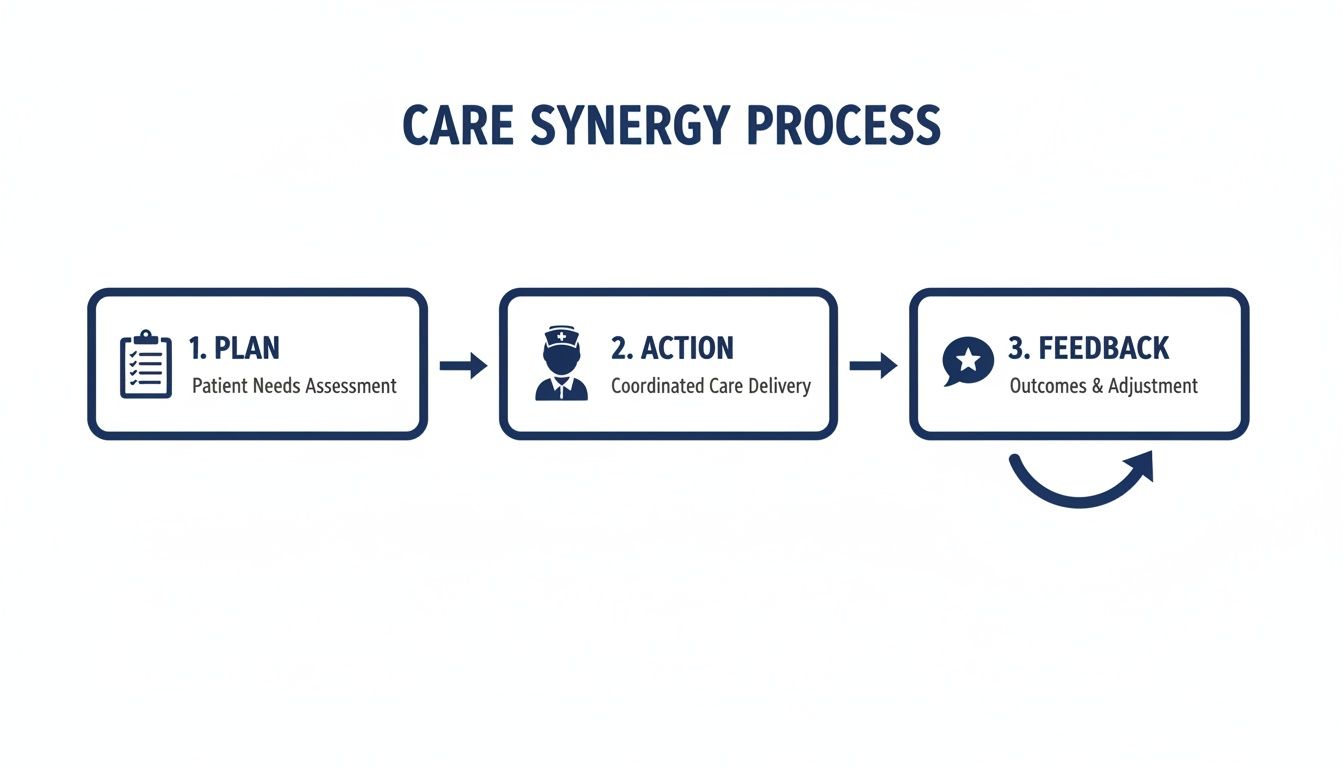
This cycle is exactly what the NDIA looks for. It shows how the funding you receive leads to real progress towards your goals.
Gathering the Right Evidence
Strong evidence is your best friend when it comes to justifying a funding request. This is where your allied health professionals become so important. Before your planning meeting, be sure to ask your therapists for formal reports or letters of support.
These documents should lay out a few key things:
- Your specific functional impairments and how they affect your day-to-day life. For instance, a report might state, "Difficulty with fine motor skills prevents the participant from being able to button their own shirt."
- The recommended therapies, including the type, how often (e.g., weekly), and for how long (e.g., over 12 months).
- A clear explanation of how these services will directly help you achieve your NDIS goals.
- Quotes for the services, which helps the planner budget accurately for your needs.
When you bring this kind of evidence to the table, you’re not just asking for funding—you’re presenting a professional, evidence-based plan for your own success. This makes it much easier for the NDIA planner to approve the "reasonable and necessary" supports you need. To see how these supports can fit into your routine, you might find our guide on assistance with daily life under the NDIS helpful.
Practical Tips for Better Care Team Communication

When everyone involved in your care is on the same page, the results are powerful. In short, good communication is the glue holding your support system together, making sure every professional is working towards your goals.
A breakdown in communication can cause confusion or missed opportunities. On the other hand, a proactive and structured approach helps your allied health providers, nursing team, and family work in harmony.
Establish a Central Communication Hub
One of the simplest yet most powerful tools is a single, agreed-upon place for all updates. This stops crucial information from getting lost in text messages or forgotten in conversation.
Choose a method that works for everyone. For some, this might be a physical communication book kept in a central spot in the home. For others, a shared digital log using a simple app is better. The key is consistency.
Practical Example: The family of an NDIS participant, Sarah, uses a dedicated notebook on her kitchen counter. After each visit, her physiotherapist jots down new exercises. Sarah’s in-home nurse then reads the entry, helps her with the exercises, and adds a note about her progress. As a result, there’s a clear record for the next physio visit.
Run Productive Team Meetings
Regular team meetings, or case conferences, are vital for aligning everyone’s efforts. This is especially true before an NDIS plan review. A good meeting ensures everyone has a voice and that decisions are made together.
Your Support Coordinator can often help run these meetings. To make them as productive as possible, it helps to have a clear agenda from the start.
A simple checklist can ensure nothing gets missed:
- Share reports beforehand: Send out any new reports from allied health services at least 48 hours before the meeting.
- Set clear goals: Begin the meeting by restating the participant's key NDIS goals.
- Review progress: Each team member should give a brief update on progress, challenges, and wins.
- Agree on next steps: End with a clear list of action items, who is responsible, and when they are due.
This structured approach makes sure everyone leaves with the same understanding and a shared plan. Having clear roles documented in your agreements also helps. You can learn more by checking out our guide on creating an NDIS service agreement template.
Why Clear Communication Is So Important
Even a small miscommunication can derail progress. Imagine a dietitian recommends a specific food thickener for someone with dysphagia. If that information isn’t clearly passed on to the in-home nurse and the family member doing the shopping, the wrong product could be bought. This creates a serious safety risk.
This is why a central communication log and regular team check-ins are so important. They create a safety net, ensuring every detail of the care plan is understood and followed correctly by everyone.
Strong partnerships between healthcare professionals are essential for delivering comprehensive care. This is especially true in areas where specialised skills are in high demand.
The uneven distribution of allied health workers across Australia adds to these challenges, with fewer professionals in rural and remote areas. Research shows that while 98% of enrolled practices engage nurses, only 28% engage allied health professionals. This gap highlights why strong communication between nursing and allied health teams is so vital for complete, coordinated care. You can discover more insights about the allied health workforce in Australia on acdhs.edu.au.
Your Top Questions About Allied Health and the NDIS
Figuring out how allied health fits into your NDIS plan can bring up a lot of questions. We get it. This final section tackles the most common queries we hear from participants and their families, with clear, straightforward answers. Our goal is to give you the confidence to make the best decisions for your care.
What’s the Difference Between Allied Health and Nursing?
It’s best to think of allied health and nursing as a partnership. One is your specialist coach, and the other is your dedicated training partner. Both roles are different, but they work together to help you succeed.
Your allied health professional is the specialist coach. They’re the expert who assesses your needs and designs a tailored program to build your skills and independence. The in-home nurse is your dedicated training partner, who’s there with you day-to-day, helping you put that program into action safely and consistently.
Here's a real-world example:
Imagine your goal is to walk more confidently after a long hospital stay.
- The Coach (Physiotherapist): A physio will visit to assess your current strength and balance. Based on that, they will create a specific set of exercises just for you.
- The Training Partner (In-Home Nurse): Your in-home nurse then helps you do these exercises every day. They make sure your technique is correct, manage any related needs like pain relief, and become the link between your therapy sessions and daily life.
How Many Therapy Hours Can I Get in My NDIS Plan?
This is a question we hear all the time, but there's no single magic number. The NDIS funds supports that are considered ‘reasonable and necessary’ to help you achieve the goals set out in your plan. The key is providing strong, clear evidence to back your request.
You need to show why a certain number of hours is needed and how those hours will lead to real results. This is where detailed reports from your allied health professionals are absolutely crucial.
The NDIA doesn't just fund activities; it funds outcomes. A well-written therapist report gives them the justification they need to approve the right level of support for you.
Let's look at an example:
An NDIS participant wants to make their own meals, but they have cognitive challenges that make following steps difficult.
- Weak Justification: "I need occupational therapy to help me in the kitchen."
- Strong Justification (from an OT report): "To achieve the goal of independent meal preparation, the participant requires 30 hours of occupational therapy over 12 months. This will be used to develop skills in planning, sequencing, and kitchen safety, with a clear plan to reduce support as skills improve."
Can I Choose My Own Allied Health Providers?
Yes, absolutely! The NDIS is built on choice and control, and we are fully committed to that principle. You always have the right to choose the providers you feel most comfortable with and who best meet your needs.
Our role is to work with your chosen team, not replace them. We see ourselves as a central hub that connects with your preferred specialists. Whether you have a team you already love or need help finding qualified providers, we will collaborate with them.
Here’s how it works:
You've been seeing the same speech pathologist for years and have a great relationship. When you start with our in-home nursing services, we’ll contact your speech pathologist (with your permission, of course) to introduce ourselves. Together, we’ll make sure the swallowing strategies they recommend are perfectly integrated into your daily mealtime support at home. It’s your team, your choice.
What If My Nurse and Therapist Disagree?
It's actually quite normal for different professionals to have different perspectives. When managed well, these discussions often lead to better and safer care plans. Think of it not as a problem, but as an opportunity to fine-tune your support.
If you notice a difference of opinion or feel the advice is conflicting, your first step should be to raise it with us or your support coordinator. Open communication is always the best way to sort these things out quickly.
Often, the most effective solution is a case conference. This is a meeting that brings everyone to the table—you, your family, your nurse, and your therapist.
Let's see it in action:
A physiotherapist recommends a new walking frame to boost independence, but your in-home nurse is concerned that your narrow hallways could make it a trip hazard.
Instead of causing confusion, a case conference is arranged. The team discusses the pros and cons. The result is a collaborative solution: the physio recommends a different, more compact walker, and the nurse agrees to hold daily practice sessions at home to ensure it can be used safely. This way, everyone is working together with your wellbeing as the top priority.
At Core Nursing Solutions Pty Ltd, we believe in collaborative, person-centred care. Our team of registered nurses and support workers is dedicated to working seamlessly with your chosen allied health services to help you achieve your NDIS goals from the comfort of your home. To learn how we can support your complex care needs in Sydney, visit us at https://corenurses.com.au.
Pingback: The Guide You Need to Empower Your Home Care Journey - Core Nursing Solutions
Pingback: Palliative Care Home Care A Guide to Compassionate In-Home Support - Core Nursing Solutions
Pingback: Palliative care in home: A Sydney Families Guide - Core Nursing Solutions