Think about what it would mean to get top-tier, hospital-grade clinical care without ever having to leave your own home. That’s the real value of a home nursing service. It’s a supportive, professional healthcare model built for NDIS participants, seniors, and anyone with complex medical needs who wants to keep living on their own terms.
What a Home Nursing Service Delivers

Essentially, a home nursing service works like a ‘hospital without walls’, bringing qualified clinical care right to your doorstep. This is an absolute game-changer for people managing long-term conditions, recovering from surgery, or needing specialised support like ventilation assistance or complex wound management.
This kind of care goes far beyond just helping with daily tasks; it’s about providing genuine medical and nursing support in a place where you feel most comfortable. For example, a nurse can administer intravenous (IV) antibiotics for a persistent infection at home, saving you from a lengthy hospital stay. This gives you the power to manage your health while holding onto your routines, dignity, and those all-important connections with family and the local community.
A Real-World Example of Home Nursing
Let’s imagine a young adult in the Wollondilly region living with a spinal cord injury. Without in-home nursing, they might face draining, time-consuming trips to a clinic every single day. Instead, a registered nurse can come to their home to provide essential catheter care. This one change frees them up to stick to their own schedule, go to TAFE or work, and spend time with friends, all while getting the expert clinical attention they need.
The demand for this kind of personalised support is on the rise. We've seen that over 280,000 Australians now have access to a Home Care Package (HCP), which is a 6% jump from the previous year. This clearly shows a major shift towards in-home support, with over 273,000 people using their packages to manage complex needs like tracheostomy care and enteral feeding from the safety of their homes.
A professional home nursing service combines clinical expertise with compassionate support, enabling individuals with complex health needs to thrive in their preferred environment—their own home.
More Than Just Medical Tasks
While clinical procedures are at the heart of what we do, a quality home nursing service is about so much more. It's a partnership, one focused on helping you reach your personal health goals and improve your overall quality of life. For example, care is often delivered hand-in-hand with specialised medical aids. It’s useful to understand what is considered durable medical equipment, as these items are often a key part of a comprehensive home care plan.
The benefits of bringing care home are clear:
- Greater Independence: You stay in control of your daily life and decisions, maintaining your autonomy. For instance, you decide when you want your wound dressing changed, fitting it around your work-from-home schedule, not a hospital's rigid timetable.
- Enhanced Comfort and Safety: Being in a familiar place reduces stress, which can make a huge difference to recovery and well-being. Our approach to home health care is built on this principle.
- Personalised Care Plans: Care is designed around your specific needs, routines, and goals, not a rigid, one-size-fits-all institutional timetable. A practical example is a nurse timing a visit to help with PEG feeding just before a client leaves for their weekly art class.
- Stronger Family Involvement: When care happens at home, it's so much easier for family to be involved and stay in the loop, creating a solid support network for everyone. A nurse might teach a family member how to confidently manage a CPAP machine's settings, empowering them to help.
Understanding Specialised In-Home Nursing Services

A professional home nursing service brings specific, high-level clinical skills right into your living room. This isn't about general support; it's about delivering specialised medical care that, not too long ago, you could only get in a hospital ward. When you understand what these services look like in daily life, you can see just how much they empower people to manage complex health needs safely and with dignity at home.
So, let's explore what this care truly involves, moving beyond the clinical jargon to see the real-world impact. Every service is provided by a qualified Registered or Enrolled Nurse who brings expertise, compassion, and a genuine focus on your personal goals. It's this personalised approach that truly transforms day-to-day life for NDIS participants and their families across Sydney and the Wollondilly.
To give you a clearer picture, here’s a breakdown of the most common specialised services we provide.
Overview of Specialised Home Nursing Services
| Service Provided | What It Involves | Example Scenario |
|---|---|---|
| Complex Wound Management | Assessing, cleaning, and dressing wounds like pressure sores, surgical incisions, or ulcers. It includes creating a care plan with a GP to promote healing and prevent infection. | An individual in Picton has a persistent pressure sore. A nurse visits 3 times a week to apply advanced dressings and track healing progress, sharing photo updates with the GP. |
| Tracheostomy & Ventilation Care | Managing breathing equipment (like CPAP/BiPAP machines or tracheostomy tubes), including suctioning, cleaning, and monitoring. A key part is teaching family members how to handle the equipment confidently. | A person in Campbelltown uses a BiPAP machine at night. A nurse visits to check settings, ensure a good mask fit, and teach their partner how to respond to alarms. |
| Enteral Feeding Support | Administering nutrition through a feeding tube (e.g., a PEG tube). This involves managing the feeding pump, flushing the tube to prevent clogs, and keeping the insertion site clean and infection-free. | A young man in the Sutherland Shire receives his nutrition via a PEG tube. A nurse visits daily to manage his feeds and educates his family on how to operate the pump safely. |
| Catheter & Bowel Care | Assisting with urinary catheters (indwelling or intermittent) and complex bowel care routines. The focus is on hygiene, infection prevention (UTIs), and maintaining comfort and dignity. | An older woman in Liverpool has an indwelling catheter. A community nurse visits regularly to change it using a sterile technique and provides advice on hydration to prevent issues. |
Each of these services is about more than just a clinical task; it's about building confidence and creating a safe, supportive environment at home.
Tracheostomy and Ventilation Care
Managing your respiratory health at home can feel like a huge responsibility, but with the right professional support, a high quality of life is absolutely achievable. This service is designed for anyone who relies on equipment to help them breathe—whether it's a tracheostomy tube, a CPAP machine, or a BiPAP machine.
A nurse doesn’t just come in to manage the equipment; they become a teacher and a source of confidence for the whole family. For example, a nurse can run a practice drill with a client's partner on how to change a tracheostomy tube tie securely, so they feel prepared for a real-life situation. They show you the ropes, answer your questions, and make sure everyone feels capable.
Complex Wound Management
Proper wound care is absolutely critical for preventing infection and helping the body heal, especially for people with limited mobility. This service goes far beyond just changing a dressing. It involves a registered nurse carrying out a full clinical assessment of the wound, creating a specific treatment plan, and monitoring progress every step of the way.
A practical example is a nurse visiting an elderly client who is recovering from surgery. The nurse not only changes the dressing on the surgical wound but also assesses the surrounding skin for signs of pressure sores and suggests repositioning techniques to prevent them.
The goal of in-home wound management is to provide consistent, expert care that accelerates healing and prevents complications, ultimately avoiding the need for hospitalisation. A nurse becomes your dedicated partner in recovery.
A qualified nurse can expertly manage a wide range of wounds, including:
- Surgical wounds following an operation
- Pressure injuries (often called bedsores)
- Diabetic ulcers
- Chronic leg ulcers
Enteral Feeding and Nutrition Support
For individuals who can't eat or drink in the traditional way, enteral feeding—often through a tube like a PEG—is a lifeline. A home nursing service ensures this process is handled safely and effectively, providing all the essential nutrition while minimising risks like infection or tube displacement.
The nurse’s support is comprehensive, covering everything from administering feeds to maintaining the equipment. For instance, a nurse might teach a client's parents how to correctly flush the feeding tube with water after each feed to prevent blockages, a simple but vital skill for maintaining the tube's function. This allows people to get the nutrition they need without being stuck in a hospital or clinic.
Catheter and Continence Management
Managing urinary catheters and bowel care requires real clinical skill to maintain hygiene, prevent infections, and ensure comfort. A home nursing service provides discreet, respectful, and professional support for these deeply personal tasks.
A practical example would be a nurse teaching a client who self-catheterises how to recognise the early signs of a urinary tract infection (UTI), such as changes in urine colour or odour, enabling them to seek prompt treatment from their GP. This kind of support is also a core part of compassionate end-of-life care, allowing individuals to maintain their dignity. You can learn more about how this is integrated into palliative care in the home and its focus on comfort.
How Do You Fund Home Nursing Care?
Figuring out the financial side of a home nursing service can feel a bit overwhelming at first, but it's really just a matter of knowing your options. Whether you're an NDIS participant or looking to pay privately, there are clear pathways to get the support you need. The trick is to understand how each system works so you can advocate for yourself or your loved one with confidence.
This is more important than ever, as more and more people are choosing to receive clinical care at home. The Australian home healthcare market, which hit USD 11.9 billion, is set to keep growing, largely thanks to an ageing population and helpful government policies. This growth is a good thing—it means more robust funding and service options are becoming available, especially for those of us here in Sydney and the Wollondilly region. You can read more about the Australian home healthcare market on imarcgroup.com.
Using Your NDIS Plan for Nursing Care
If you're an NDIS participant, your plan is your key to unlocking funding for in-home clinical support. Generally, nursing services will fall under two main budget categories in your plan:
- Core Supports: This is your flexible funding for daily living. A practical example would be using this funding for a nurse to manage daily insulin injections because a participant's vision impairment prevents them from doing it safely themselves.
- Capacity Building Supports: This budget is all about developing your independence. For instance, this funding could cover a nurse who teaches a young person with a new PEG tube how to manage their own feeds, empowering them for the future.
The National Disability Insurance Agency (NDIA) needs a solid reason to fund these services. It’s not just a matter of asking for a nurse; you have to show them exactly why this clinical support is "reasonable and necessary" for managing your disability-related health needs.
To get nursing care approved, you need to draw a clear line connecting the service directly to your disability. The NDIA wants to see that this support is essential for you to live safely at home and work towards your goals.
A Real-World Example: Justifying NDIS Funding
Let’s imagine someone living in Camden who needs overnight ventilation support (BiPAP). Their Support Coordinator would be instrumental in pulling together the right evidence to show the NDIA at their next plan review.
Here’s how that process would unfold:
- Get the Specialist Reports: First, the Support Coordinator would get a formal letter from the person’s respiratory specialist. This report needs to clearly state why the BiPAP is medically necessary and spell out the risks if their breathing isn't properly managed.
- Detail the Exact Support Needed: The report must be specific, explaining that a trained nurse is needed to watch over the equipment all night, handle any alarms, and provide immediate help if something goes wrong.
- Link It to NDIS Goals: Finally, all this evidence is tied directly to the participant's NDIS goals, like "to live independently at home" or "to maintain my health and well-being."
When you present a strong, evidence-based case like this, it’s no longer just a request—it becomes a clear, critical need in the eyes of the NDIA. To dig a bit deeper into this, have a look at our guide on NDIS in-home care for more detailed information.
Private Funding and Other Avenues
If you aren't an NDIS participant, paying privately is the most direct way to organise a home nursing service. This path gives you total control and flexibility over the care you receive, with no need to meet government eligibility criteria.
When you're paying privately, make sure you ask for a detailed quote and a clear service agreement upfront. For example, if you need a nurse to visit twice a week for wound care, the agreement should explicitly state the cost per visit, any travel fees, and the price of specific dressing materials. This document should break down all the costs, the exact services you'll be getting, and the care schedule, so there are absolutely no surprises down the track.
How Quality Care Is Coordinated
Great home nursing care isn't something that just happens. It's a carefully managed team effort, with a lot of work going on behind the scenes to make sure everything runs smoothly. Think of it like a skilled orchestra conductor ensuring every instrument plays in harmony. In a home nursing service, a Registered Nurse often takes on that conductor role, acting as the central care coordinator to bring all the different pieces of your healthcare puzzle together.
Understanding what is care coordination in healthcare is the key to seeing how this structured approach leads to better results for you. It's all about being proactive—managing your health, preventing unnecessary hospital trips, and helping you hit your personal goals while living comfortably at home.
And it all starts not with a prescription pad, but with a conversation.
The In-Home Assessment and Care Plan
The very first step is a thorough in-home assessment. A Registered Nurse will visit you at home to understand more than just your clinical needs. They want to get the full picture: your personal goals, your daily routines, and what a good quality of life truly looks like to you.
This isn’t just a medical check-up. It's a collaborative session where you and your family are the experts on your own life.
- Here’s a real-world example: Imagine a resident in the Wollondilly area recovering from a major operation. The coordinating nurse will ask about their mobility goals, like wanting to walk to the local shops again. They’ll also chat about the practical challenges, such as navigating stairs or staying on top of pain medication.
From this detailed assessment, the nurse develops a person-centred care plan. This document is essentially the roadmap for your care, outlining every specific action, from medication schedules to wound dressing procedures. And it's a living document—it gets reviewed and updated regularly as your needs evolve.
The Hub of Communication: Your GP and Specialists
A quality home nursing service acts as the central communication hub between you, your GP, and your specialists. The coordinating nurse makes sure everyone is on the same page, preventing the kind of fragmented care that happens when different health professionals work in silos.
This constant communication loop is vital. For example, if a nurse notices a change in your blood pressure readings during a visit, they'll immediately get in touch with your GP to discuss a potential medication adjustment. Another practical example is a nurse sending a photo of a healing wound to a client's wound specialist to get expert advice without needing an extra appointment. This proactive approach helps nip issues in the bud before they become serious problems.
A coordinated care model turns reactive healthcare into proactive support. Instead of just treating symptoms as they appear, the entire team works together to anticipate needs and prevent complications.
The infographic below illustrates how different funding streams come together to make this coordinated care possible.
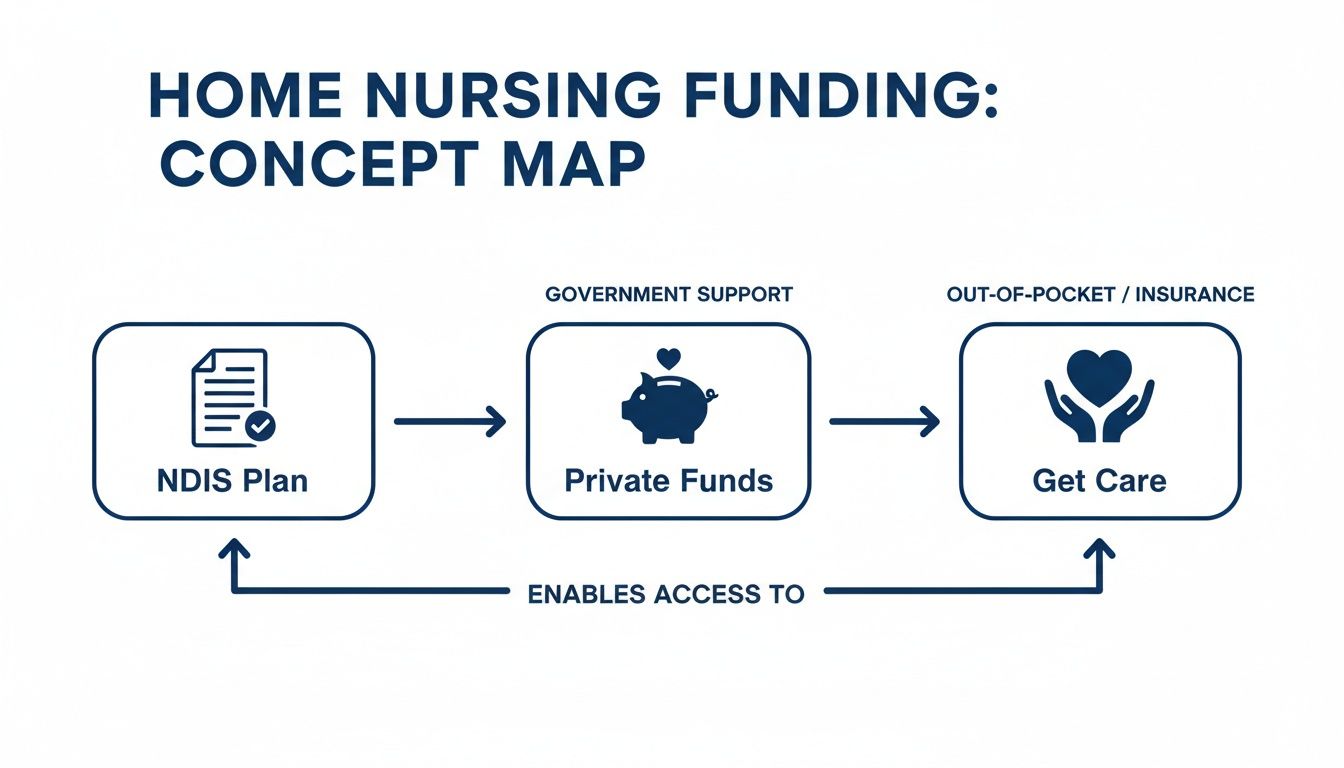
This visual shows that whether you're using your NDIS plan or private funds, the end goal is always the same: receiving high-quality, person-centred care that works for you.
Collaborating with Allied Health Professionals
Your health is about much more than just medical tasks. It involves your physical movement, speech, nutrition, and overall well-being. That's why strong collaboration with allied health professionals is a non-negotiable part of any great home nursing service.
The coordinating nurse works hand-in-hand with specialists to create a single, unified approach to your health.
- Physiotherapists: The nurse can reinforce exercises prescribed by a physio, ensuring you’re performing them correctly and safely between visits. For instance, the nurse can observe the client doing their daily leg stretches and provide feedback to the physio.
- Occupational Therapists: If an OT recommends specific equipment to make daily tasks easier, the nurse ensures it’s used properly and to its full benefit. A practical example is a nurse showing a client how to correctly use a shower chair recommended by the OT to prevent falls.
- Dietitians: For someone with enteral feeding needs, the nurse works closely with a dietitian to monitor nutritional intake and tolerance, making adjustments as needed. For example, the nurse might report back to the dietitian that a client is experiencing bloating, prompting a change in the feeding formula.
This teamwork ensures every piece of your care plan supports your bigger health goals. You can learn more about how we integrate with allied health services to deliver truly holistic support. By coordinating every element, a home nursing service helps you not just manage a condition, but genuinely thrive at home.
Choosing the Right Home Nursing Provider in Sydney
Picking a home nursing provider is a massive decision, one of the most important you’ll make for yourself or a family member. The right team does so much more than just clinical tasks; they become genuine partners in your health journey. With so many options out there across Sydney and Wollondilly, it’s vital you know how to spot a provider who is not only skilled but also reliable and compassionate.
This isn't just about looking at a website and ticking a few boxes. It's about digging a bit deeper and asking the right questions. You need to feel completely confident that the team you choose can handle complex health needs with the highest level of professionalism and care.
Core Credentials and Qualifications
First things first: let's talk about the absolute non-negotiables. You have to verify the qualifications of any provider you’re considering. Don’t just assume everyone is operating at the same standard, because they aren't.
Here are the essential questions you need to ask from the get-go:
- Are all your nurses registered with AHPRA? In Australia, every single nurse providing clinical care must be registered with the Australian Health Practitioner Regulation Agency (AHPRA). This isn't optional; it's the absolute baseline for professional practice.
- What specific training do your staff have for complex needs? If you need support with things like ventilation, complex wounds, or enteral feeding, ask them to get specific. For example, ask: "Can you provide a practical example of the training your nurses receive for managing a PEG tube?"
- Are you a registered NDIS provider? For anyone using NDIS funding, this is crucial. A registered provider has passed the NDIS Commission's strict quality and safety audits.
A good sign of a provider’s commitment to quality is their membership in industry bodies like the Australian Community Industry Alliance (ACIA). It shows they’re serious about upholding best practices and ethical standards.
Evaluating Safety and Emergency Protocols
A key part of a quality home nursing service is how they handle the unexpected. You need absolute certainty that there are solid systems in place to keep you or your loved one safe, especially when managing serious health conditions.
Don't be shy about asking direct questions about their safety procedures:
- What happens if there's a medical issue after hours? There should be a crystal-clear, documented plan. Who is the on-call contact? What are the steps for escalating a situation if it becomes serious?
- How do you handle and report clinical incidents? A professional organisation will have a transparent system for reporting incidents. A practical example is asking them how they would handle a situation where a client had a fall during a nurse's visit.
- What are your infection control policies? This has always been important, but now more than ever. Staff should be following strict hygiene and infection control protocols every single time they visit.
A provider’s approach to safety and emergencies speaks volumes about their professionalism. If you get vague or uncertain answers to these questions, consider it a major red flag.
The demand for these services is putting a real strain on the system, making your choice even more critical. Projections show that while over 530,000 Australians will need home care, only about 299,765 government-funded packages will be available. This gap really highlights the urgent need for dependable, high-quality providers you can trust. You can read more about the rising demand for home care on lumiacare.com.au.
Communication and Collaboration
Finally, great care is built on clear and consistent communication. The provider you choose should be an active partner, one who works closely with you, your family, and your entire healthcare team, including your GP and other specialists.
Here are some final things to consider:
- How will you communicate with our GP and allied health team? Look for a provider who takes the initiative to build those relationships and provide regular, meaningful updates. For instance, do they use a secure messaging app or provide written reports?
- Can we be involved in creating and reviewing the care plan? A person-centred approach isn't just a buzzword. It means you are at the heart of every decision. Your input should be actively welcomed and valued.
- Who is our main point of contact? Knowing you have a dedicated care coordinator or case manager to call with questions makes all the difference.
To help you through this process, we've put together a simple checklist with key questions to ask potential providers. It’s designed to help you compare your options and find the best fit.
Provider Selection Checklist: Questions to Ask
| Category | Key Question to Ask | Why This Is Important |
|---|---|---|
| Credentials & Staffing | Can you confirm all your nurses are AHPRA-registered and have experience with my specific needs? | Ensures a baseline of professional, legal, and competent clinical practice. |
| Care Planning | How will I and my family be involved in developing and reviewing my care plan? | A person-centred approach is vital. The care must be tailored to your goals and preferences, not the provider's. |
| Safety & Emergencies | What is your protocol for after-hours emergencies or if a regular nurse is sick? | You need a reliable plan for unexpected events to ensure continuity and safety of care at all times. |
| Communication | How do you communicate with my GP and other allied health professionals? | Good care is coordinated. The provider should be a proactive part of your wider healthcare team, not a silo. |
| Fees & Funding | Can you provide a clear, itemised quote and explain how you manage NDIS or private funding? | Avoids hidden costs and financial surprises. A transparent provider will be upfront about all charges. |
Choosing the right partner is a big step, but by being prepared and asking these questions, you can make a decision with confidence. A well-informed choice brings real peace of mind, knowing you’ve found a team truly dedicated to providing safe, compassionate, and high-quality care.
For a deeper dive into what to expect from providers, check out our guide on home care services in Sydney.
Taking the Next Steps to Arrange Care
Taking that first step from learning about home nursing services to actually getting care organised can feel like a huge leap. We get it. That's why we've made our process as straightforward and supportive as possible, so you feel understood and in control right from the start.
It all begins with a simple phone call or a message through our website. This first chat is really just a conversation—a chance for you to tell us a bit about your situation, ask any pressing questions, and see if we feel like the right fit for you and your family. We'll listen first, then ask for some basic details to get the ball rolling, like your general location in the Sydney or Wollondilly area and the type of clinical support you're looking for.
Your Initial Consultation and Assessment
After our first chat, the next step is to book a thorough assessment in your own home with one of our senior Registered Nurses. We'll find a time that works for you. This meeting is much more than just a clinical tick-and-flick; it’s our chance to properly meet you, understand your personal goals, and see how your home environment can best support your health.
To help make this meeting really count, it’s a good idea to have a few things handy:
- Your NDIS Plan: If you're an NDIS participant, having your plan details on hand helps us align the services with your approved funding.
- Medical Information: A list of your current medications, any formal diagnoses, and the contact details for your GP and other specialists is incredibly helpful.
- Your Key Goals: Have a think about what a successful outcome looks like for you. Is it about becoming more independent? Better pain management? Or maybe it's simply staying out of hospital. For example, a practical goal could be: "I want to be able to manage my own wound dressing within three months."
This assessment is the cornerstone of your entire care plan. We're not here to tell you what you need; we're here to listen to what matters most to you and build a support system around those priorities.
This collaborative discussion is what allows us to map out a truly personalised care plan. It's a clear, practical document that details the specific nursing tasks, visit schedules, and how we'll all communicate, so everyone is on the same page. Our goal is to make the entire process of starting home nursing feel seamless and reassuring.
Ready to talk? Contact us today to begin the conversation.
Your Home Nursing Questions, Answered
When you're thinking about bringing a nurse into your home, it's natural to have questions. It’s a big decision. Here are some straightforward answers to the things we get asked most often, designed to give you clarity and confidence.
Are Your Nurses Qualified for Complex Care?
Yes, they absolutely are. Our team is made up of experienced Registered Nurses who have specific, hands-on training in complex care. We're talking about specialised skills like managing tracheostomies, providing ventilation support (CPAP/BiPAP), and handling intricate wound dressings.
We don't just stop at initial qualifications, either. Every nurse on our team is committed to ongoing professional development, keeping their skills sharp and up-to-date with the latest best practices. A practical example of this is our nurses completing an annual competency assessment for catheterisation to ensure their technique remains sterile and safe. This means you can be confident that the care you or your family member receives is not just compassionate, but also meets the highest clinical standards for safety.
How Is a Home Nurse Different From a Support Worker?
This is a really important question, as the two roles are quite different but often work side-by-side. Think of it this way: a support worker is there to help with the activities of daily life—things like helping with showers, preparing meals, or getting out into the community. They provide essential, practical help.
A home nursing service, on the other hand, delivers clinical care that, by law, must be performed by a Registered or Enrolled Nurse. This includes medical tasks like giving injections, managing catheters, operating specialised equipment, and assessing complex health conditions. For example, a support worker can remind a client to take their medication, but only a nurse can administer an insulin injection.
A support worker helps you live your life, while a nurse provides the medical care you need to stay healthy and safe at home. Often, the best support plans involve both working together as a team.
What Happens in a Medical Emergency?
Your safety is always our first priority, without exception. Before we even begin, we work with you to create a detailed care plan that includes a crystal-clear emergency protocol. For instance, for a client with epilepsy, the plan would detail the specific steps the nurse must take during a seizure, including timing it, ensuring the client's airway is safe, and knowing when to call an ambulance. Our nurses are fully trained in first aid and how to respond calmly and effectively when things go wrong.
In any critical situation, their immediate action is to call for an ambulance (000) to get you the urgent medical help you need. As soon as it's safe to do so, they will contact your designated family member and your GP, making sure everyone who needs to be is kept in the loop. We have solid procedures in place to manage any emergency professionally and safely.
Can We Request a Specific Nurse for Our Care?
We know how much comfort and trust comes from having a familiar face. Building that relationship is a huge part of what we do. While it's not always possible to guarantee the exact same nurse for every single visit due to rosters and availability, we make continuity of care a massive priority.
Our approach is to assign a small, core team of nurses to each client. For example, instead of having ten different nurses visit over a month, you might have a primary team of two or three who share the visits. This way, you'll always have someone you know and trust, who understands your personal preferences and clinical needs inside and out. We always do our best to accommodate your requests and focus on finding the right match in both skill and personality, ensuring you feel consistently supported.
Ready to talk about how professional, compassionate home nursing could make a difference for you or your loved one? The team at Core Nursing Solutions Pty Ltd is here to listen and help you arrange the support you need. Find out more on our website
Pingback: A Guide to Private Nursing Care in Home for Sydney Residents - Core Nursing Solutions