Palliative care at home is a specialised approach that puts your quality of life front and centre, all within the familiar comfort of your own home. It’s not just about end-of-life care; it's a supportive layer that helps manage symptoms, reduce stress, and maintain dignity right from the moment of diagnosis. For instance, someone undergoing chemotherapy for cancer might receive palliative care to manage treatment side effects like nausea and fatigue, allowing them to continue their daily life more comfortably.
What In-Home Palliative Care Really Means

It’s easy to think of palliative support as something reserved for the final days of life, but that’s a common misunderstanding. A better way to see it is as an extra layer of support that works right alongside curative treatments. It’s a proactive service, designed to help you handle the physical and emotional challenges of a serious illness so you can feel comfortable and in control at every stage.
The real goal is to help you or your loved one live as well as possible, for as long as possible. This becomes especially powerful when that care is delivered at home, the one place where we all feel most secure.
The Comfort of Familiar Surroundings
There’s a deeply human need to be in our own space, surrounded by the people and things we love. This isn't just about sentiment—it has a genuine impact on wellbeing. For many, the idea of a sterile, impersonal hospital setting only adds to the anxiety of being unwell. For example, being able to sleep in your own bed, eat meals in your own kitchen, or have a pet curled up beside you can significantly reduce stress and promote a sense of calm.
This is a feeling shared right across the country. While a staggering 70% of Australians with a terminal illness say they want to spend their final days at home, the reality is that only 15% get to do so. This gap highlights just how vital it is to have strong, reliable home-based services that can bridge the divide between clinical needs and personal comfort.
Palliative care at home allows you to keep your own routines, stay connected with your community, and hold onto a sense of independence. It shifts the focus from simply treating an illness to caring for the whole person.
Bridging Clinical Care and Emotional Support
Bringing palliative care into a home environment takes a unique blend of clinical skill and genuine compassion. It’s about having hospital-level expertise right in your living room, making sure that symptoms like pain, breathlessness, or anxiety are managed effectively and promptly. A practical example is having a registered nurse visit to adjust pain medication in real-time, based on your reported comfort levels, rather than waiting for a doctor's appointment.
It's a space where providers like Core Nursing Solutions truly shine, especially for NDIS participants from Sydney to Wollondilly. We focus on creating a supportive environment that honours a person’s dignity and choices above all else. For families exploring this option, a helpful family guide to end of life care at home can offer some valuable insights.
Ultimately, the aim is to make high-quality, person-centred home health care accessible, so you can remain where you feel safest and most loved.
What Services Are Included in Home Palliative Care
Knowing that palliative care in home is all about quality of life is one thing. Seeing what that support actually looks like day-to-day is another. It’s never just a single service; it's a coordinated effort from a whole team of professionals, brought together to meet your specific physical, emotional, and practical needs.
This team typically includes your GP, registered nurses, and trained support workers, all working in sync. The idea is to create a seamless care experience so you receive consistent, high-quality support without ever having to leave your house. For example, after a nurse's visit, they might coordinate directly with your GP to get a new prescription filled and have a support worker pick it up, all without you having to manage the logistics.
Think of it as a comprehensive safety net, addressing everything from complex medical issues to the simple human need for comfort and dignity. It’s about bringing the right skills and compassion directly to your doorstep.
A well-rounded home palliative care plan is comprehensive, covering a wide range of needs. To give you a clearer picture, here’s a look at the core services you can expect.
Core Services in Home-Based Palliative Care
| Service Category | Description | Practical Example |
|---|---|---|
| Symptom Management | Proactive clinical care to manage pain, nausea, breathlessness, and other distressing symptoms. | A nurse adjusts medication to relieve pain and teaches breathing techniques to manage anxiety. |
| Complex Nursing Tasks | Specialised clinical procedures that would otherwise require a hospital visit. | Managing a complex wound, changing a catheter, or providing tracheostomy care. |
| Personal Care | Dignified assistance with daily activities like showering, dressing, and mobility. | A support worker helps you get ready for the day safely and comfortably. |
| Psychosocial Support | Emotional, spiritual, and social support for you and your family to reduce stress and isolation. | Connecting with a counsellor, arranging for spiritual guidance, or simply having a trusted professional to talk to. |
| Equipment & Aids | Arranging and managing necessary medical equipment, like hospital beds or oxygen concentrators. | Organising the delivery and setup of an adjustable bed to improve comfort and mobility at home. |
| Care Coordination | Liaising with your GP, specialists, and other health providers to ensure seamless, integrated care. | A nurse communicates with your doctor after observing a change in your condition, ensuring the care plan is updated promptly. |
Each of these elements works together, creating a holistic support system that adapts to your changing needs.
Clinical Nursing and Symptom Management
A huge part of in-home palliative services is managing symptoms that cause distress and discomfort. This is where the clinical expertise of a registered nurse is absolutely essential. They are trained to assess and respond to a whole range of physical challenges. For instance, if you're experiencing severe nausea, a nurse can administer anti-sickness medication via injection for fast relief and then work with your doctor to find a longer-term oral solution.
This proactive approach aims to get symptoms under control before they become overwhelming, which can make a world of difference to your day-to-day life. It allows you to focus more on your family and what matters to you, and less on the illness itself.
Specialised and Complex Nursing Tasks
Beyond general symptom control, many people need specialised clinical support to stay safely at home. In-home palliative care teams are equipped to handle complex nursing tasks that might otherwise mean a trip to the hospital. A practical case would be a patient who requires intravenous (IV) antibiotics; instead of a lengthy hospital stay, a qualified nurse can administer the IV treatment at home each day.
These services make sure that even people with high-level needs can get the right care in a familiar, comfortable setting. It’s a huge part of maintaining independence and avoiding disruptive hospital admissions.
Core Nursing Solutions provides skilled nurses for a range of these tasks, including:
- Wound Care: Managing complex or chronic wounds to prevent infection and help them heal.
- Medication Administration: Safely giving medications, including injections or infusions.
- Catheter and Bowel Care: Assisting with urinary catheters and complex bowel management routines.
- Ventilation Support: Caring for individuals who use CPAP, BiPAP, or other non-invasive ventilators.
- Tracheostomy Care: Offering specialised support for maintaining a tracheostomy tube.
These specialised services are the bridge that allows hospital-level care to be delivered with the compassion and familiarity of home. They empower individuals to stay where they feel most comfortable, without compromising on clinical safety.
Psychosocial and Emotional Support
A serious illness affects more than just the body. It takes a toll on your emotional, social, and spiritual wellbeing, too. A truly holistic palliative care plan addresses these needs for both you and your family. It’s about caring for the whole person, not just the diagnosis. For example, a care provider might notice a family caregiver is struggling and arrange for respite care, giving them a few hours off to recharge, or connect them with a local caregiver support group.
This support can be as simple as having a trusted professional to talk to, or as structured as coordinating with counsellors and spiritual advisors. The goal is to reduce feelings of isolation, anxiety, and stress that often come with a serious illness. It also extends to helping families navigate the huge challenges of being a caregiver.
To see how different professionals contribute, you can learn more about our allied health services and the role they play in a complete care team.
Ultimately, palliative care is designed to be flexible and responsive. By combining expert clinical skills with genuine emotional support, this approach helps ensure your time at home is as comfortable, dignified, and meaningful as it can possibly be.
The Real Benefits of Choosing Care at Home

The decision to arrange palliative care in home goes so much deeper than just medical treatment. It’s a choice that brings profound emotional and psychological benefits, not only for the person receiving care but for their entire family. This approach puts comfort, dignity, and personal choice front and centre in a way that clinical settings often can't.
At its heart, home-based care is about holding onto a sense of normalcy and control. Being surrounded by familiar sights, sounds, and the simple rhythm of home life provides an incredible source of comfort during what can be a very challenging time. It allows people to stay in the place where they’ve built memories, feel safest, and can simply be themselves.
Maintaining Dignity and Independence
One of the most powerful advantages of receiving care at home is the ability to maintain independence and personal dignity. Even when managing a serious illness, being able to make small, everyday choices—like what to have for dinner, when to get up, or who comes to visit—is incredibly empowering.
Think of it this way: a hospital has to run on its own schedule, but a home runs on yours. This simple shift in control can dramatically reduce feelings of helplessness. For example, a patient might choose to have their personal care assistance in the late morning because they've always enjoyed a slow start to their day, a preference that would be difficult to accommodate in a hospital. This simple choice reinforces their sense of self.
This person-centred approach is a core principle here at Core Nursing Solutions. We truly believe that empowering someone to live on their own terms is just as important as managing their clinical symptoms.
The Comfort of Familiar Surroundings
There is a powerful, almost therapeutic, quality to being at home. It’s where your favourite chair is, where family photos line the walls, and where you can look out at your own garden. These simple comforts create a peaceful environment that can significantly lower stress and anxiety.
Another huge benefit is reducing the need for frequent, and often draining, hospital visits. Avoiding the logistics of travel and the clinical atmosphere of a hospital ward means more energy can be devoted to what truly matters—spending quality time with loved ones. For instance, instead of travelling to an outpatient clinic for a dressing change, a nurse performs the task at home, saving the patient's limited energy for a video call with their grandchildren later that day.
By bringing expert care into the home, you transform the environment from a place of potential stress into a sanctuary of comfort. It allows for a greater sense of peace and stability for everyone involved.
Australia's ageing population is creating a growing need for more accessible end-of-life care options. With the number of people aged 85 and over projected to triple between 2025 and 2045, the demand for palliative services is set to increase significantly. Yet, access is still a challenge; in one recent year, only 4,800 of 245,000 people entering aged or home care were even assessed for palliative needs. The data shows that individuals receiving home care are twice as likely to access these vital services, which really highlights the critical role it plays. You can explore more data on Australia's palliative care needs to see the full picture.
Enabling Deeper Family Involvement
When care happens at home, it naturally becomes a more shared, inclusive experience. Family members and close friends can be more actively involved in the day-to-day journey—not just as visitors during set hours, but as true partners in care.
This involvement strengthens relationships and provides mutual support. It allows for more spontaneous moments of connection, whether it’s sharing a meal, watching a movie, or simply being present together in a quiet room. Our care team can also teach family members simple techniques to help with comfort—such as how to safely reposition someone in bed to relieve pressure—making them feel more confident and less like bystanders.
Here’s how it empowers families:
- Shared Decision-Making: Families can participate more directly in discussions with nurses and doctors.
- Reduced Caregiver Stress: Professional support at home eases the emotional and physical burden on family caregivers.
- Creating Lasting Memories: It provides the time and space to create meaningful final memories together in a familiar, private setting.
Ultimately, choosing palliative care in home offers a path that honours personal wishes and strengthens family bonds. The team at Core Nursing Solutions is dedicated to supporting Sydney families through this journey, ensuring our home care services in Sydney deliver both clinical excellence and heartfelt compassion.
Navigating NDIS and Other Funding for Palliative Care
Working out the financial side of palliative care can feel overwhelming, but understanding your options is the first step towards getting the right support in place. When it comes to palliative care in home, it’s less about finding a single source of funding and more about weaving together different programs to create a complete safety net.
Think of it like putting together a puzzle. Each piece—the NDIS, Medicare, and other government programs—covers a different part of the picture. Knowing how they fit together allows families and support coordinators to build a plan that truly meets every need.
Leveraging Your NDIS Plan
For NDIS participants, your plan is a powerful resource for funding many aspects of in-home palliative support. While the NDIS doesn't directly pay for clinical health treatments (that’s the health system's job), it absolutely covers the disability-related supports that help you manage daily life and stay comfortable at home.
This means your NDIS plan can fund the practical, hands-on help you need to maintain your independence, manage your environment, and get assistance with personal activities. The entire focus is on supporting you to live as comfortably and autonomously as possible in your own space.
For example, while Medicare covers your GP appointments, the daily assistance from a skilled support worker or nurse to help manage your condition at home can often be funded through your NDIS plan.
Here are a few real-world examples of how NDIS funding can be used:
- Complex Bowel Care: Your Core Supports budget can fund a support worker to assist with your daily bowel management routine.
- Enteral Feeding Assistance: If you rely on a feeding tube, your plan can cover a trained professional to help manage feeds and maintain the equipment.
- Seizure Management: Funding can be allocated for a support worker to monitor for seizures and provide immediate assistance based on your management plan.
- Personal Care: Assistance with showering, dressing, and moving around helps you conserve energy and remain comfortable, all of which can be claimed under Core Supports.
Exploring all the available support for NDIS participants is a great way for families to ensure they’re building a truly comprehensive care plan.
The Role of Medicare and Other Programs
Beyond the NDIS, Australia's broader health system provides the essential funding for the medical side of palliative care. This is mainly handled through Medicare, ensuring you always have access to the clinical services you need.
Medicare is the foundation of your medical care, covering services from your doctors and specialists. This is crucial for a holistic approach, making sure clinical oversight works hand-in-hand with your daily in-home support.
Think of it like building a house: Medicare provides the essential framework of doctors and medical advice, while your NDIS plan can provide the internal supports—like skilled assistants and daily help—that make the house liveable and comfortable.
Here’s a look at how these funding streams work together.
Funding Pathways for In-Home Palliative Care
This table breaks down the main funding options, what they typically cover, and who can access them, helping you see how a complete support package comes together.
| Funding Source | What It Covers | Primary Eligibility |
|---|---|---|
| NDIS | Disability-related supports for daily living, personal care, and community participation. | Australian citizens/residents under 65 with a permanent and significant disability. |
| Medicare (MBS) | Consultations with GPs, specialists, and some allied health professionals. | All Australian citizens and permanent residents. |
| Government Programs | Subsidised medicines (PBS), and sometimes specific state-based palliative care programs. | Varies by program, often based on medical need. |
By taking a collaborative approach, we can ensure that both your clinical and your personal care needs are fully met.
For more detail on how an NDIS plan can be structured for day-to-day assistance, you can explore our specific NDIS in-home care services. When you understand how each piece of the funding puzzle fits, you can confidently arrange the comprehensive, person-centred care you deserve.
How to Arrange In-Home Care with Core Nursing Solutions
Taking that first step to arrange professional palliative care in home can often feel like the most difficult part. When you’re dealing with a serious illness, the last thing you need is a confusing or complicated process. At Core Nursing Solutions, we’ve made our approach as straightforward and supportive as we possibly can. We want you to feel heard, respected, and in control right from the very first chat.
The journey usually starts with a simple phone call or a referral from your GP, hospital, or support coordinator. This first contact is a chance for you to share your story and for us to simply listen. We want to understand what you need right now, what your worries are, and what a good day looks like for you. For example, you might tell us, "My main concern is managing my dad's pain overnight so he can sleep," which immediately gives us a clear, practical starting point.
This is much more than just a logistical chat; it’s about starting a relationship built on genuine trust and understanding. We believe exceptional care begins with a conversation, not a checklist.
The In-Home Assessment and Planning
After our initial discussion, we’ll arrange a thorough in-home assessment. This is a really important step where one of our senior registered nurses will visit you in your own environment. It’s a relaxed, collaborative meeting that includes you, your family, and anyone else you’d like to have in the room.
During this assessment, our goal is to build a complete picture of your needs, and that goes far beyond a clinical diagnosis.
We talk about your personal goals, what your daily routines are like, and any cultural or spiritual preferences you have. This deep level of understanding allows us to create a care plan that’s not just medically sound but truly person-centred, reflecting who you are and what matters most to you.
This first assessment is the bedrock of a dynamic care plan. Our nurse will pinpoint specific support needs—from symptom management to help with daily activities—and explain exactly how our team can step in. For instance, they might notice that the bathroom layout could pose a fall risk and immediately suggest installing a shower chair and grab rails, which we can help arrange. It’s an open dialogue where you can ask anything and voice any anxieties, making sure you feel completely comfortable moving forward.
Collaborating with Your Healthcare Team
Seamless care is all about teamwork. The relationships you already have with your GP and other specialists are incredibly important, and our job is to strengthen that network, not replace it. We work hand-in-glove with your entire healthcare team to make sure everyone is on the same page.
This collaboration means your care stays consistent and perfectly coordinated.
- Regular Communication: We keep the lines of communication wide open with your doctors, giving them updates on your condition and working together on any adjustments to your care plan.
- Shared Goals: We make sure our in-home support aligns with the medical goals set by your specialists, ensuring our work complements any ongoing treatments.
- Unified Support: This approach stops any conflicting advice and ensures every member of your support network is pulling in the same direction—towards your comfort and wellbeing.
This infographic shows our simple, clear process for getting care started, from that first call right through to the beginning of your support.
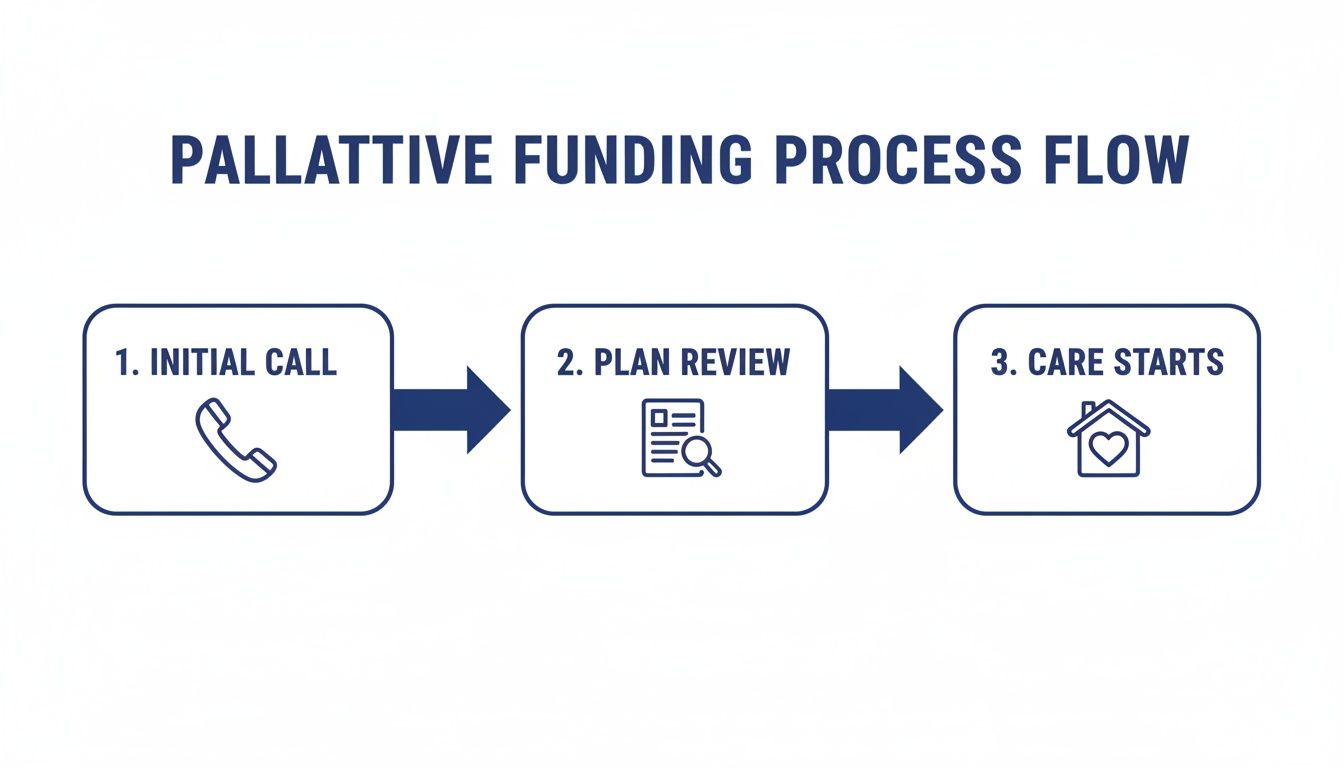
As you can see, each step flows logically into the next. It’s all designed to make the journey into care as smooth and stress-free as possible.
Respecting Cultural and Spiritual Needs
Providing care that truly honours your personal beliefs is at the heart of what we do. We know that cultural, spiritual, and personal values play a huge part in a person's sense of wellbeing and peace, especially when facing a serious illness.
Our team takes the time to ask about and understand what is important to you and your family. Whether it involves specific dietary practices, religious observances, or family traditions, we weave these elements respectfully into the care plan. A practical example could be scheduling personal care times to not interfere with daily prayer or ensuring that meals prepared by our support workers adhere to specific religious dietary laws, like Halal or Kosher. This commitment ensures the support you receive feels authentic to you.
The process of arranging palliative care in home should empower you, not overwhelm you. Our structured, yet flexible, approach is designed to take the uncertainty out of the equation and build a foundation of trust. If you're ready to learn more about our specific support options, you can explore our full range of services and see how we can assist you and your family.
Your Questions About In-Home Palliative Care, Answered
Deciding on palliative care in home is a big step, and it's completely normal to have a lot of questions. For most people, it's new territory. We find that having clear, straightforward answers helps families feel more confident and in control.
Below, we’ve put together some of the questions we hear most often from families across the Sydney to Wollondilly region. Our hope is to clear up any confusion and show you just how supportive this type of care can be, giving you the clarity you need to move forward.
When Is the Right Time to Start Palliative Care?
This is easily the most common question we get, and the simple answer is often "sooner than you might think." There's a persistent myth that palliative care is strictly for the very end of life. In reality, its benefits are greatest when it's introduced early on, sometimes right from the day of diagnosis.
Starting early gives the care team a chance to build a genuine, trusting relationship with you and your family. More importantly, it allows us to get ahead of symptoms like pain, breathlessness, or anxiety before they become overwhelming. For example, someone with early-stage Chronic Obstructive Pulmonary Disease (COPD) might begin palliative care to learn breathing techniques and energy conservation strategies that improve their daily life long before their condition becomes advanced.
The best time to start talking about palliative care is when a serious illness begins to affect your daily comfort and quality of life. The goal is to get support in place so you can live as well as possible, for as long as possible.
Can I Still See My Own Doctors and Specialists?
Absolutely. In fact, it’s essential. In-home palliative care is designed to work alongside your existing healthcare team, not replace it. Your GP and specialists know your medical history inside and out, and they are crucial partners in your care.
Think of our registered nurses and support workers as your hands-on team at home. We complement the fantastic work your doctors are already doing by being their eyes and ears on the ground. We communicate regularly with your GP, sharing observations and reporting any changes so your care plan can be adjusted quickly. This teamwork creates a seamless, coordinated approach where everyone is pulling in the same direction for your health and comfort.
Here’s how that partnership looks in a real-life scenario:
- During a home visit, one of our palliative care nurses might notice a new or worsening symptom.
- They’ll immediately get in touch with your GP to discuss what they’ve seen.
- Together, they might decide to adjust your medication or change part of your daily care routine.
- That change is then put into practice straight away, often avoiding a stressful trip to the hospital.
What’s the Difference Between Palliative Care and Hospice Care?
It’s easy to get these two confused, but there’s one key difference. Palliative care can be provided at any stage of a serious illness, often at the same time as treatments aimed at a cure, like chemotherapy or dialysis. The primary goal is always to manage symptoms and provide support, no matter the long-term outlook.
Hospice care, on the other hand, is a specific type of palliative care for people who are nearing the end of their life and are no longer receiving curative treatments. So, while all hospice care is palliative, not all palliative care is hospice. You could receive palliative support for many months or even years to help you manage your condition and live more comfortably.
How Is the Family Involved in Palliative Care at Home?
Family isn't just involved—they are at the very heart of everything we do. Effective in-home palliative care simply doesn't work without you and your loved ones being central to every conversation and decision. Our team makes a point of working closely with your family to understand their needs, worries, and questions, because they need support, too.
This support can look like a few different things:
- Education: We can teach family members practical skills for providing daily comfort, which helps them feel more empowered and less like bystanders.
- Respite: Our services can give family carers a much-needed break to rest and recharge, confident that their loved one is in safe, professional hands.
- Emotional Support: Sometimes, what’s needed most is a listening ear. We’re here to help families navigate the emotional journey of caring for someone with a serious illness.
By supporting the entire family unit, we help foster a more stable, calm, and loving environment at home for everyone. This holistic approach ensures that palliative care in home actually strengthens family bonds during what can be an incredibly tough time.
At Core Nursing Solutions Pty Ltd, our team is ready to answer any other questions you have and help you navigate your care options with compassion and confidence. If you're in the Sydney to Wollondilly area and think our in-home support could be right for you or your family, please get in touch with us today. Find out more about how we can help by visiting us at https://corenurses.com.au.