Imagine bringing the clinical expertise you'd find in a hospital right into the comfort and familiarity of your own home. That’s the heart of private nursing care—it’s skilled medical support from a Registered Nurse, specifically designed to manage complex health needs safely and effectively. This is a world away from general home help.
Defining In-Home Clinical Expertise
Private nursing care at home delivers professional medical services, the kind you’d normally only get in a clinic, directly to your doorstep. We’re not talking about companionship or help with household chores; this is about high-level clinical care managed by qualified and registered nurses.
Think of it like this: a personal support worker is fantastic for helping with daily activities like showering and preparing meals. But a private nurse steps in when tasks require real medical training and credentials. For instance, a support worker can remind your father to take his blood pressure medication, but a registered nurse is qualified to administer his insulin injection, assess the injection site for issues, and adjust the dosage according to the doctor's sliding scale based on his blood sugar reading. Their job is to manage the complex health issues that allow someone to stay safely at home, rather than in a hospital or specialised facility.
What Does This Care Look Like?
The scope of private nursing is incredibly broad because it’s always shaped around your specific medical needs. The focus is on maintaining your health, preventing complications, and keeping you as independent as possible.
Some of the key services include:
- Complex Medication Management: This is far more than just a reminder to take a tablet. It involves administering injections, managing intravenous (IV) lines, and closely monitoring for any side effects from new medications. For example, a nurse would manage a portable IV pump for a patient receiving antibiotics at home, ensuring the correct flow rate and checking the line for signs of infection or dislodgement.
- Advanced Wound Care: A registered nurse can properly assess and treat complex or chronic wounds, like surgical incisions or pressure sores. They use specialised dressing techniques to stop infection in its tracks and promote healing. A practical example is a nurse using a vacuum-assisted closure (VAC) dressing on a diabetic foot ulcer, a complex procedure that actively promotes healing.
- Chronic Disease Support: For ongoing conditions like diabetes, respiratory disease, or epilepsy, a nurse provides the monitoring, education, and intervention needed to manage symptoms and prevent things from escalating. For someone with COPD, this could involve teaching them correct inhaler techniques, checking their oxygen saturation levels, and recognising the early signs of a chest infection.

This level of professional oversight is absolutely crucial. It’s the difference between simply living at home and thriving at home, knowing that clinical risks are being properly managed by an expert.
It also means that small but significant changes in your health get picked up on and dealt with straight away, which can often prevent a trip back to the hospital. For instance, a nurse might notice a slight increase in swelling in a client's legs, recognise it as a potential sign of worsening heart failure, and immediately contact their GP for a medication review.
This proactive, skilled approach is what quality in-home nursing is all about. You can learn more about how these services fit into the bigger picture by exploring community nursing frameworks. The ultimate goal is always the same: to create a safe, responsive, and dignified healthcare experience, right where you feel most comfortable.
What Does In-Home Nursing Actually Involve?
The real difference with private nursing care at home is the sheer scope of clinical services a Registered Nurse (RN) can bring right to your doorstep. This isn't just a watered-down version of hospital care. It’s highly specialised, one-on-one medical support that’s built around a person's specific health needs, their personal goals, and the reality of their own home.
We’re moving far beyond basic help here. This is about tackling complex, often life-sustaining, health challenges with genuine skill and compassion. It’s all focused on managing health conditions, heading off potential problems, and helping people live safely and with dignity at home.
Let’s break down what that looks like on a day-to-day basis.
Complex Medical and Personal Support
This is where the high-level clinical skills of a nurse truly shine. These are the kinds of tasks that, for safety and legal reasons, can only be handled by a qualified and registered nurse. They demand expert knowledge, a steady hand, and critical thinking.
Tracheostomy and Ventilation Management: For anyone breathing with a tracheostomy tube or a ventilator (like a CPAP or BiPAP machine), a nurse's care is absolutely vital. They aren't just there to watch the equipment. They perform sterile suctioning to keep the airways clear, provide regular site care to stop dangerous infections, and know exactly how to respond to alarms or any sign of breathing difficulty. For example, a nurse managing a client's overnight ventilation in their Sydney home makes sure the mask fits just right to prevent pressure sores and that oxygen levels are stable, giving the whole family peace of mind to get a good night's sleep.
Enteral Feeding (PEG/NG Tube): When someone can't eat or drink safely, a feeding tube might be necessary. A private nurse manages the entire process—administering the specialised feed and medications through the tube, and just as importantly, keeping the site meticulously clean to prevent skin breakdown and infection. A practical example is flushing the tube with water before and after each feed to prevent blockages, a simple but critical step that ensures the person receives their nutrition without complications.
Advanced Continence and Catheter Care: This is about so much more than just managing symptoms; it’s about protecting health and preserving dignity. An RN is trained to manage indwelling catheters (IDCs) and suprapubic catheters (SPCs), handling changes with a sterile technique that dramatically cuts the risk of urinary tract infections (UTIs)—a very common reason for ending up back in hospital.
Bringing this level of care into the home is a huge step forward. The demand for private nursing in Australia shows just how important this is. Managing chronic diseases, for instance, made up around 32.27% of private nursing revenue in a recent year. This shows the clear need for skilled nurses to look after conditions like heart failure, COPD, and diabetes outside of a hospital setting. To see the full picture of what’s possible, you can find more detail on our community nursing services.
Clinical Nursing vs Personal Care: A Clear Comparison
It’s easy to get confused between the roles of a Registered Nurse and a Support Worker. A nurse handles complex clinical tasks, while a support worker focuses on daily living and personal assistance. Think of it as the difference between medical treatment and essential daily support.
This table breaks it down:
| Service Category | Clinical Nursing Care Examples (Registered Nurse) | Personal Care Examples (Support Worker) |
|---|---|---|
| Medication | Administering injections, managing IV lines, complex medication schedules, monitoring for side effects. | Reminding to take tablets, assisting with opening packets. |
| Wound Care | Assessing and treating complex wounds like surgical sites, diabetic ulcers, or pressure sores with advanced dressings. | Applying simple creams or basic dressings to minor cuts. |
| Continence | Changing indwelling or suprapubic catheters, managing complex stomas, bladder washouts. | Assisting with continence pads, helping to get to the toilet. |
| Feeding | Managing PEG/NG tube feeds, assessing swallow safety (dysphagia). | Preparing meals, assisting with eating and drinking. |
| Mobility | Assessing skin integrity, managing specialised equipment, developing pressure area care plans. | Assisting with transfers (e.g., bed to chair), helping with walking. |
Both roles are crucial for holistic in-home care, but they meet very different needs. A great care plan ensures you have the right person for the right task.
Chronic Disease Management
Living with a long-term health condition at home needs consistent, expert oversight. A private nurse becomes your health coach, your clinical watchdog, and a direct line to your GP and specialists. Their job is to keep things stable and prevent the flare-ups that can lead to an emergency.
Having a dedicated nurse for chronic disease management means someone is consistently tracking the small changes that often signal a bigger problem. This proactive approach is key to avoiding preventable hospital visits.
Let’s take 'David', a resident in the Wollondilly area with Type 2 diabetes and a history of slow-healing foot ulcers. His private nurse visits three times a week. She doesn't just change the wound dressing; she reviews his blood sugar logs, discusses his diet, checks his feet for any new pressure spots, and makes sure he's using his insulin correctly. This constant, expert support helps keep his blood sugar on track and his wound healing, preventing a potentially limb-threatening infection.
This kind of management includes:
- Diabetes Management: Giving insulin injections, checking blood glucose levels, and providing practical education on diet and lifestyle to keep things stable. A nurse might show a newly diagnosed patient how to correctly rotate injection sites to prevent skin damage or help them understand how different foods impact their sugar levels.
- Complex Wound Care: Assessing and treating chronic wounds—like pressure injuries, venous ulcers, or tricky surgical sites—using advanced dressing techniques to speed up healing.
- Epilepsy and Seizure Support: Being ready to administer emergency medication and putting seizure management plans into action to keep the person safe. This includes timing the seizure, ensuring the person's airway is clear, and administering medication like Midazolam if required by their care plan.
- Medication Management: This is far more than just a reminder service. It involves giving injections, juggling complex medication timings, and watching for side effects and drug interactions, all while liaising directly with the doctor. For instance, a nurse can manage a complex post-transplant medication regimen, ensuring anti-rejection drugs are taken at the exact right time and blood levels are monitored correctly.
By bringing this level of clinical skill into the home, private nursing makes it possible for people with even the most challenging health conditions to live with more independence, security, and a better quality of life.
Navigating NDIS and Other Funding Options
Figuring out how to pay for private nursing care at home can feel like the biggest hurdle, but there are a few clear pathways available. For many people across Sydney with complex health needs, the National Disability Insurance Scheme (NDIS) is the main source of funding for this kind of essential clinical support.
To successfully use your NDIS funding, you need to show that the nursing care is both ‘reasonable and necessary’ to manage your disability-related health needs. It’s not designed for general healthcare that the public system would normally cover. Instead, it’s for specific, ongoing support that helps you live safely at home and be part of your community. For example, ongoing care for a spinal cord injury is disability-related, whereas short-term nursing after a routine appendix operation would likely be covered by the health system.
Using Your NDIS Plan for Nursing Care
NDIS funding for nursing usually falls into two main budget categories. Which one is right for you depends entirely on the type of support you need and how intensive it is.
- Capacity Building – Improved Daily Living: This budget is often tapped into for nursing supports that are more therapeutic or training-focused. A nurse might, for example, work with you to build your confidence and skills in managing your own diabetes, or they might train your support workers in specific procedures related to your care, like how to properly operate a hoist.
- Core Supports – Assistance with Daily Life: This is where the funding for more hands-on, high-intensity nursing tasks typically comes from. If you need a nurse for regular catheter changes, complex wound dressing, or ventilation support, the funding will almost certainly be allocated from your Core budget.
Making a strong case for this support in your NDIS planning meeting is absolutely critical. You have to clearly connect the nursing hours you're requesting directly to your disability needs and personal goals.
The key is to provide solid evidence. This means getting reports from your GP, specialists, and allied health therapists that specifically recommend in-home nursing and clearly explain why it's essential for your health and wellbeing.
This simple decision tree can help you figure out if your needs are clinical or more personal.
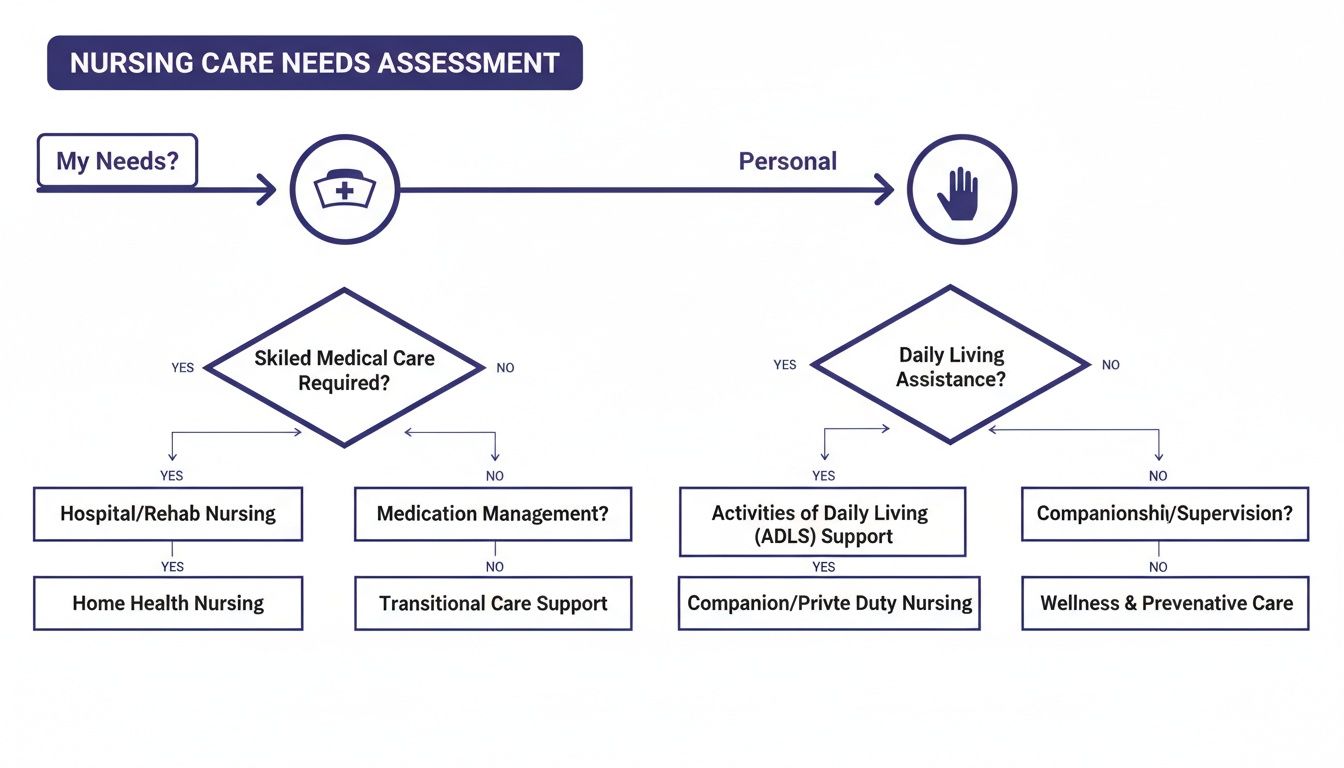
As the flowchart shows, clinical needs require a Registered Nurse, while personal care needs can be met by a support worker. This distinction is what guides your funding requests.
A Practical Sydney Scenario
Let’s look at a real-world example. A person living in Sydney has complex respiratory needs and requires overnight ventilation to breathe safely. Without this support, they would face constant hospital visits and their quality of life would be seriously impacted.
- Preparation: They work with their Support Coordinator to get a detailed report from their respiratory specialist. This report outlines exactly why 24/7 nursing oversight is a medical necessity.
- Planning Meeting: In the NDIS meeting, they present this evidence, explaining that constant monitoring is a disability-related need, not just a standard health service.
- Outcome: The NDIS planner agrees the support is reasonable and necessary. Funding is approved under Core Supports, covering the costs for a dedicated team of nurses to provide round-the-clock private nursing care at home.
Exploring Other Funding Pathways
While the NDIS is a major pathway, it isn't the only one. Knowing all your options helps you build a care plan that’s sustainable for the long term.
- Private Health Insurance: Some top-level hospital policies include benefits for ‘hospital in the home’ or nursing care after an operation. It's really important to check your specific policy, as this cover is often limited to short-term recovery periods, for instance, a two-week period of daily wound care after a knee replacement.
- My Aged Care: For Australians over 65, a Home Care Package (HCP) can be used to fund nursing services. The assessment process is different from the NDIS, but it offers a government-subsidised way for older people to get clinical support to stay at home.
- Self-Funding: Paying privately gives you the most flexibility and lets you access services immediately, without having to meet strict eligibility rules. This is often the best solution for people who don't qualify for other schemes or just need to top up their existing funded support.
These systems can feel complicated to get your head around, but with the right preparation and advocacy, you can secure the funding you need for high-quality clinical care. For more practical advice on setting up your support, you can find more in-depth information in our articles that explore different aspects of in-home care.
What Are the Real-World Benefits of In-Home Clinical Care?

Choosing clinical care at home goes far beyond simple convenience. It’s a decision that genuinely enhances quality of life, improves health outcomes, and brings an incredible sense of relief to everyone involved. The positive effects really do ripple through every part of a person's recovery and daily life.
To really get what this means, let's paint a picture. Imagine 'Sarah', a resident in the Wollondilly area who’s just come home after complex surgery. Leaving the hospital was terrifying. She had a new pain management pump she didn't understand, a complicated wound dressing, and a medication schedule that looked like a timetable. The thought of something going wrong meant a long, stressful trip right back to the hospital.
But instead, a dedicated registered nurse came to her home every day. This consistent, professional support completely changed her recovery. The nurse didn't just change the dressing; she was an expert pair of eyes, watching for the first subtle signs of infection. She liaised with Sarah's GP to fine-tune her pain relief and made sure the medication schedule was followed perfectly. This proactive care kept Sarah safe, comfortable, and—most importantly—at home, where she belonged.
Comfort and Dignity in Your Own Space
There's something incredibly powerful about healing in your own home. Being in your own bed, surrounded by familiar things and with family or pets close by, dramatically reduces stress and anxiety. We know that stress gets in the way of recovery, so this comfort isn't a luxury; it’s a crucial part of getting better.
When private nursing care at home is an option, it means people can stick to their own routines and keep a sense of control over their lives. For example, instead of being woken at 6 a.m. for a hospital ward's medication round, a person can arrange for their nurse to visit at a time that suits their own sleep schedule. For someone recovering from an operation or managing a chronic illness, that feeling of normality is absolutely vital for their emotional and mental health.
A person-centred approach means that care fits into your life, not the other way around. It’s about receiving expert clinical support without having to sacrifice the comfort and security of being at home.
This deep desire to remain at home is what drives in-home care in Australia. With more than 280,000 Australians receiving government-funded Home Care Packages, it's clear people want to stay in their own communities. As millions more Australians get older, projections show the national system might struggle to keep up. This makes private nursing services, from Sydney to the Wollondilly Shire, absolutely essential to fill the gaps. You can dive deeper into the home care statistics in Australia to see the full picture.
Better Health Outcomes and Fewer Risks
The clinical benefits of at-home care are significant and well-proven. One of the biggest advantages is the drastically lower risk of picking up a hospital-acquired infection. Even with the best hygiene, hospitals are environments where superbugs can linger.
Receiving care at home means you avoid that exposure—a critical factor for anyone with a compromised immune system or post-surgical wounds. What's more, having the same nurse visit you means they get to know your personal health baseline inside and out. They are in the perfect position to spot tiny changes that might signal a problem, allowing for early intervention that can prevent a serious complication or another trip to the hospital.
Key health benefits include:
- Reduced Infection Rates: Simply by avoiding exposure to hospital-borne pathogens.
- Lower Hospital Readmissions: Proactive monitoring and quick action stop small issues from becoming big ones. For instance, a nurse can teach a heart failure patient to weigh themselves daily. A sudden weight gain can signal fluid retention, allowing the nurse to alert the GP for a medication adjustment before breathing difficulties lead to an ER visit.
- Improved Medication Adherence: One-on-one time with a nurse ensures you understand what you're taking and why, making treatments more effective.
- Greater Family Involvement: It's easier for family to be part of the care journey, learning how they can help and providing that irreplaceable emotional support.
At the end of the day, this kind of personalised, one-on-one attention from a skilled nurse creates a safer recovery. It leads to better health results and empowers people like Sarah to confidently get their independence back in the one place they feel most secure: their home.
How to Choose the Right Nursing Provider in Sydney
Choosing a provider for private nursing care at home is one of the most critical decisions your family can make. This isn't just about ticking boxes on a checklist; it's about inviting a team into your home to manage complex, often delicate, health needs. You're placing your trust in their skill, compassion, and reliability.
Finding the right partner for this journey means looking past the glossy brochures and asking the tough questions. You need to understand their real commitment to quality and safety. Here’s a practical framework to help you find a top-tier nursing provider in the Sydney to Wollondilly region.
Verify Essential Credentials and Governance
First things first, let’s cover the non-negotiables. Any legitimate, professional provider will have their credentials and policies ready to share. If they don’t, that’s a major red flag.
Your initial checklist should include:
- NDIS Registration: Is the provider registered with the NDIS? This is your guarantee that they meet the strict quality and safety standards mandated by the NDIS Commission.
- Clinical Governance Framework: Ask to see their clinical governance policy. This document is their playbook for ensuring safe, high-quality care, managing risks, and constantly improving how they do things. A practical example of this in action is their procedure for reporting and investigating medication errors to prevent them from happening again.
- ACIA Membership: Being a member of an industry body like the Australian Community Industry Alliance (ACIA) shows a provider is serious about upholding ethical standards and best practices.
Think of these as the foundations of a house. Without them, everything else is unstable. A provider who is transparent and proud of these credentials is one you can start to build trust with.
Dig Deeper with Specific Questions
Once the basics are confirmed, it's time to see how their expertise plays out in the real world. Vague questions get vague answers. You need to ask targeted questions that truly test their processes and the skill of their nursing team.
Don't just ask, "Are your staff qualified?" Instead, try asking, "What specific, hands-on training do your nurses have for managing complex ventilation, and how do you regularly check their competency with that equipment?"
See the difference? This level of detail separates an average provider from an exceptional one. Here are a few more powerful questions you can adapt:
- For Complex Care: "Can you talk me through your exact protocol for responding to a blocked PEG tube or a ventilator alarm at 2 AM?"
- For Staff Training: "How often do your nurses get updated training on advanced wound care or the latest continence management products?"
- For Communication: "How do your nurses document and share updates with our GP and allied health team after each visit? Can I see what a sample report looks like?"
The answers you get will tell you everything you need to know about the depth of their clinical expertise and their commitment to ongoing staff education—both of which directly affect the quality of care you’ll receive.
Assess Their Collaborative Approach
Brilliant private nursing care at home never happens in a silo. The best providers act as the central coordinator for your entire medical team, working seamlessly with your GP, specialists, and allied health professionals. This ensures everyone is on the same page, working towards the same health goals.
Ask potential providers how they make this collaboration happen. Do they organise case conferences? What secure digital platforms do they use to share progress notes? A provider with a proven track record of strong partnerships with local Sydney and Wollondilly healthcare professionals is set up to deliver truly holistic and coordinated care. For instance, a good provider will have a clear process for contacting a client's physiotherapist to report a change in mobility or a new pain symptom, ensuring the therapy plan can be adjusted quickly.
Australia’s long-term care system supports over 1.2 million people, but it’s no secret that workforce shortages are a major challenge. Many facilities are finding it hard to meet the required nursing targets. This is where specialised private nursing teams add incredible value—they can reliably deliver high-acuity, collaborative care right in your home, easing the strain on the broader healthcare system.
Making the right choice comes down to finding a team with not just the clinical skills, but also the communication and organisational backbone to become a true partner in your health journey. If you have more questions or want to chat about your specific needs, feel free to get in touch with our expert team for guidance.
Common Questions About Private Home Nursing
Stepping into the world of private nursing care at home often brings up a lot of practical questions. We find that families across Sydney and the Wollondilly region want to feel confident and clear about what to expect, and that's exactly what this section is for.
Here are some straightforward answers to the queries we hear most often, designed to give you peace of mind as you make these important decisions.
How Is a Private Nurse Different from a Carer?
The main difference comes down to their qualifications and the specific tasks they are legally and professionally allowed to do. It’s all about clinical skill and registration.
A Registered Nurse (RN) has a university degree and is licensed to manage complex clinical care. This means they can handle things like giving injections, managing advanced wound dressings, operating medical equipment like ventilators, and making qualified judgements about a person's health.
A carer, or support worker, is there to provide that vital non-clinical help with daily life. Their focus is on personal care—assisting with showering and dressing, preparing meals, providing companionship, or helping with transport.
To put it in perspective: a support worker can help someone eat their meal, but only a Registered Nurse can safely manage a PEG feeding tube or assess a person's swallowing to prevent choking. A great provider makes sure these two roles work together seamlessly, creating a complete circle of support.
What Happens if My Medical Needs Suddenly Change?
This is one of the biggest strengths of having professional private nursing care at home—the built-in ability to spot changes and respond quickly. It’s not just about reacting; it’s about having a plan for the unexpected.
Our nurses are trained to pick up on subtle signs that a person's health might be shifting. It could be a small change in breathing, a new patch of red skin, or a wound that looks a little different from yesterday.
When a nurse notices a change, a clear clinical process kicks in immediately:
- The observation is thoroughly documented.
- They get in touch with your GP or specialist straight away.
- They work with the wider medical team to formally update your care plan.
This system is designed to prevent emergencies before they even start. For instance, by spotting the early signs of a urinary tract infection, a nurse can contact the GP for prompt treatment at home, often preventing a painful condition and a trip to the hospital.
How Does an In-Home Nurse Work with My GP?
Collaboration is the absolute foundation of excellent in-home nursing. Your private nurse becomes the critical link between what’s happening at home and your broader medical team—your GP, specialists, and allied health professionals like physiotherapists.
This partnership is built on clear, consistent communication.
You can think of the in-home nurse as your GP's eyes and ears on the ground. They provide the real-time clinical observations that allow your doctor to make the best possible decisions for your care, even when you can't make it to the clinic.
This happens in a few practical ways:
- Secure Updates: After important visits, nurses send secure digital reports to your GP, keeping your medical records completely up to date.
- Photo Documentation: For wound care, a nurse might send a secure photo of a healing wound to a specialist. This allows for an expert assessment without you having to travel.
- Case Conferences: The nurse can join case conferences, either in person or over telehealth, to discuss your progress and help create a unified care strategy.
They also reinforce the work of other health professionals. If a dietitian sets a new meal plan, the nurse helps you stick to it. If a physio gives you exercises, the nurse can support you to do them safely. It ensures everyone is on the same page, working towards your health goals.
Is 24/7 Private Nursing Care Available in Sydney?
Yes, absolutely. For individuals across Sydney and Wollondilly with high-intensity or complex medical needs, comprehensive 24/7 private nursing care at home is available. This level of support is always structured around your specific clinical requirements and funding.
This could mean a dedicated team of nurses working in coordinated shifts for someone who needs overnight ventilation to breathe safely, or for someone requiring continuous palliative care to manage their symptoms. It guarantees there is always a skilled professional on hand for monitoring and immediate help.
The care is completely flexible. It can be scaled up or down as your needs evolve, from a one-hour daily visit for medication to round-the-clock support. This adaptability means even those with the most complex conditions can receive safe, professional, and dignified care in the comfort of their own home, day or night. To learn more about how we structure our services, you can explore the full range of options at Core Nursing Solutions Pty Ltd.
At Core Nursing Solutions Pty Ltd, our team of Registered Nurses and skilled support workers is dedicated to providing compassionate, expert care in your home. If you have more questions or wish to discuss your unique needs, please visit us at https://corenurses.com.au.
Article created using Outrank