Disability home care isn’t just about having someone pop in to help out. It’s a genuine partnership designed to empower individuals to live with independence and dignity in their own homes. This support goes far beyond basic medical aid, blending hands-on personal care for daily routines with skilled clinical care from nurses for more complex health needs. Generally speaking, it’s all built around you and your personal goals. For instance, a goal might be to attend a weekly community garden club. The service would then provide the specific support needed—like mobility assistance and transport—to make that happen.
Demystifying Disability Home Care

When people hear “Disability home care,” they often picture simple companionship or a bit of help with the chores. But true disability home care offers a much deeper, more holistic level of support. It’s a person-centred approach that completely rejects any one-size-fits-all model. Instead, it’s about creating a support system that’s as unique as the person it’s for.
Think of it like getting a vehicle customised. A standard car might get you from A to B, but it won’t work for everyone. Someone might need special hand controls to drive, a ramp for wheelchair access, or specific navigation tech. In the same way, disability home care builds a support plan around an individual’s specific needs, lifestyle, and what they want to achieve. For example, a person who loves cooking but has limited hand strength might get support that includes pre-chopped vegetables and adapted utensils, enabling them to continue their passion safely.
The Two Pillars of Disability Home Care
At its heart, disability home care stands on two distinct but connected pillars: personal care and clinical care. Getting your head around the difference is key to seeing the full picture of support available.
- Personal Care is all about assistance with activities of daily living (ADLs). On the whole, this is the practical, hands-on help that makes a real difference in maintaining independence and quality of life day-to-day. For example is a support worker assisting someone to have a shower and get dressed in the morning, respecting their choices on what to wear.
- Clinical Care covers the medical tasks that have to be done by a qualified health professional, like a registered nurse. This is absolutely essential for managing complex health conditions safely at home. For instance, a nurse might visit to administer medication via an injection or change a catheter.
For example, a support worker providing personal care might help someone with mobility challenges get dressed and make breakfast. Later that day, a registered nurse could visit to provide clinical care, perhaps managing a complex wound or administering specialised medication. Both roles are vital cogs in a single, cohesive care plan.
A Partnership Focused on Your Goals
Ultimately, the real aim of disability home care services is empowerment. As a result, it makes it possible for individuals to live the life they choose, in the comfort and familiarity of their own home.
This might mean supporting someone to join a community art class, helping them manage a chronic health condition without constant hospital stays, or simply ensuring they can get through their daily routine with confidence and dignity. For example, if a person’s goal is to manage their own budget, a support worker might help them set up online banking and practice using it weekly until they feel confident on their own.
The essence of quality home care is its collaborative nature. It is not something done to a person, but rather something done with them—a partnership built on trust, respect, and a shared commitment to achieving personal goals.
This partnership approach has never been more important. Recent data shows a growing gap in service availability across Australia. In 2022, a concerning 39.4% of people with disabilities under 65 reported needing more formal assistance than they were getting.
This statistic really highlights the critical need for responsive and reliable providers like Core Nursing Solutions. We serve communities from Sydney to Wollondilly by tailoring support to meet these essential needs. You can explore more about these trends on the Australian Bureau of Statistics website.
The Spectrum of Support Available in Disability Home Care
Disability home care isn’t just about having someone pop in; it’s about bringing professional, coordinated support right into the comfort and familiarity of your own home. This is about more than just convenience. It’s about creating a plan that works with your life, your routines, and your personal space.
The support we can offer is incredibly broad, covering everything from complex medical procedures that require a nurse, to the essential hands-on help that makes each day run a little smoother.
Think of it like this: on one end of the spectrum, you have highly specialised clinical care delivered by a registered nurse. On the other, you have personal support focusing on daily living activities, provided by a fantastic support worker. Both are vital, and together they create a complete in-home care solution that champions your independence.
Clinical Nursing Care: High-Acuity Support at Home
For anyone with significant health needs, the idea of managing everything at home can feel overwhelming. But that’s exactly where our skilled clinical care comes in.
A registered nurse can manage a wide range of medical tasks that are crucial for your health and wellbeing. In short, their job is to deliver treatments, keep a close eye on your condition, and step in proactively to make sure small issues don’t become big problems.
Here are just a few real-world examples of what this clinical support looks like:
Clinical Support At Home
- Ventilation Support: Our nurses can manage non-invasive ventilation gear like CPAP or BiPAP machines. They’ll ensure the settings are right and monitor your breathing to prevent any complications. For instance, they might perform a nightly check-in to ensure the mask fits correctly and that oxygen saturation levels are stable.
- Complex Wound Management: If you’re recovering from surgery or dealing with a chronic wound, a nurse provides expert care. This includes dressing changes, watching for infection, and using advanced techniques to help you heal. As a practical example, a nurse may use a specialised vacuum-assisted closure (VAC) dressing for a slow-healing leg ulcer.
- Tracheostomy Care: This requires absolute attention to detail. A nurse handles routine cleaning, suctioning, and any emergency procedures, giving you and your family total peace of mind. This could involve teaching a family member the correct, sterile technique for suctioning.
- Enteral (Tube) Feeding: Managing PEG or nasogastric tubes involves the precise administration of nutrition and medication. It’s a task our qualified nurses handle with skill and care. An example is flushing the tube before and after each feed to prevent blockages.
These aren’t just clinical tasks; they are lifelines. They empower people with complex needs to not just live, but thrive at home. Having this level of professional nursing care on hand is fundamental. To get a better sense of these specialised services, you can learn more about the different types of community nursing services available and see how they can be adapted to your specific needs.
Personal Care: Assisting with Daily Life
While clinical care handles the medical side of things, personal care focuses on the activities of daily living. It’s the practical, hands-on support that helps you maintain your dignity, independence, and quality of life. Additionally, our support workers are trained professionals who build relationships based on trust and respect.
This support is always person-centred—which is just our way of saying it’s all about you. We deliver it according to your schedule and your preferences.
The goal of personal care is never to take over, but to empower. It’s about giving you the right amount of help at the right time, so you can live as self-sufficiently as you choose.
Here’s how this works in practice:
- Mealtime Support for Dysphagia: For someone with swallowing difficulties, a support worker can help prepare textured meals and ensure you’re using safe eating techniques. Most importantly, it’s all about making mealtimes safe and enjoyable again. A practical example is preparing a pureed meal and adding thickener to drinks to achieve the correct consistency prescribed by a speech pathologist.
- Mobility Assistance: Our team can help you move safely around your home. Whether it’s helping you transfer from a bed to a wheelchair or just offering a steadying arm during a walk, we’re there to reduce the risk of falls. This could involve using a hoist for transfers, ensuring safety straps are correctly fastened every time.
- Personal Hygiene: This can include help with showering, getting dressed, and grooming. Everything is delivered with the utmost respect for your privacy and dignity. For instance, a support worker might lay out two outfit choices to ensure the person still has control over what they wear.
To make the distinction clearer, this table gives a simple overview of how these two types of care complement each other.
Comparing Clinical and Personal Care Support
| Type of Support | Examples of Services | Provided By |
|---|---|---|
| Clinical Care | Medication management, complex wound dressing, catheter care, ventilation support, tracheostomy management. | Registered Nurse (RN) or Enrolled Nurse (EN) |
| Personal Care | Assistance with showering and dressing, meal preparation, mobility support, light domestic tasks, companionship. | Trained Support Worker or Personal Carer |
When you bring them together, clinical and personal care create a truly robust support system. Furthermore, this integrated approach ensures every part of your wellbeing is looked after—from complex health conditions to your daily comfort—making home the best possible place for you to be.
Navigating the NDIS for Disability Home Care Needs
For many Australians, the National Disability Insurance Scheme (NDIS) is the key to unlocking the funding needed for disability home care. Getting your head around it can feel like a huge task, but the secret is to stop seeing your NDIS plan as a set of rigid rules. Instead, think of it as a flexible budget, designed to help you build the life you want.
It’s a bit like being handed a toolkit. Inside, you’ve got different tools (your funding categories) that are perfect for specific jobs (the support services you need). Your role, along with your support network, is to pick the right tools to achieve your personal goals. When it comes to home care, the most useful tools are usually found in your Core Supports and Capacity Building budgets.
Understanding NDIS Support Categories for Disability Home Care
Your NDIS plan organises your funding into three main buckets. Depending on how they help you meet your goals, both personal and clinical home care can be paid for from these budgets.
- Core Supports: This is your most flexible funding, meant for the day-to-day things. It covers help with self-care activities like showering and dressing, household chores, and getting out and about in the community. For example, if you need a hand with preparing meals or moving safely around your house, the funding would come from your Core Supports budget, specifically under “Assistance with Daily Life”.
- Capacity Building: This funding is all about investing in you. It’s there to help you build your skills, confidence, and independence for the long haul. A great example is using Capacity Building funds for a therapist to teach you safer ways to move around your home, which could reduce your need for hands-on physical support over time. For example, an occupational therapist might teach you how to use a shower chair and grab rails to shower independently.
- Capital Supports: This category is for bigger-ticket items, like specialised equipment or changes to your home. In other words, if you needed a specialised bed, assistive technology, or a wheelchair ramp installed, the funding would come from Capital Supports. A practical example is funding the installation of a ceiling hoist to make transfers between bed and wheelchair safer.
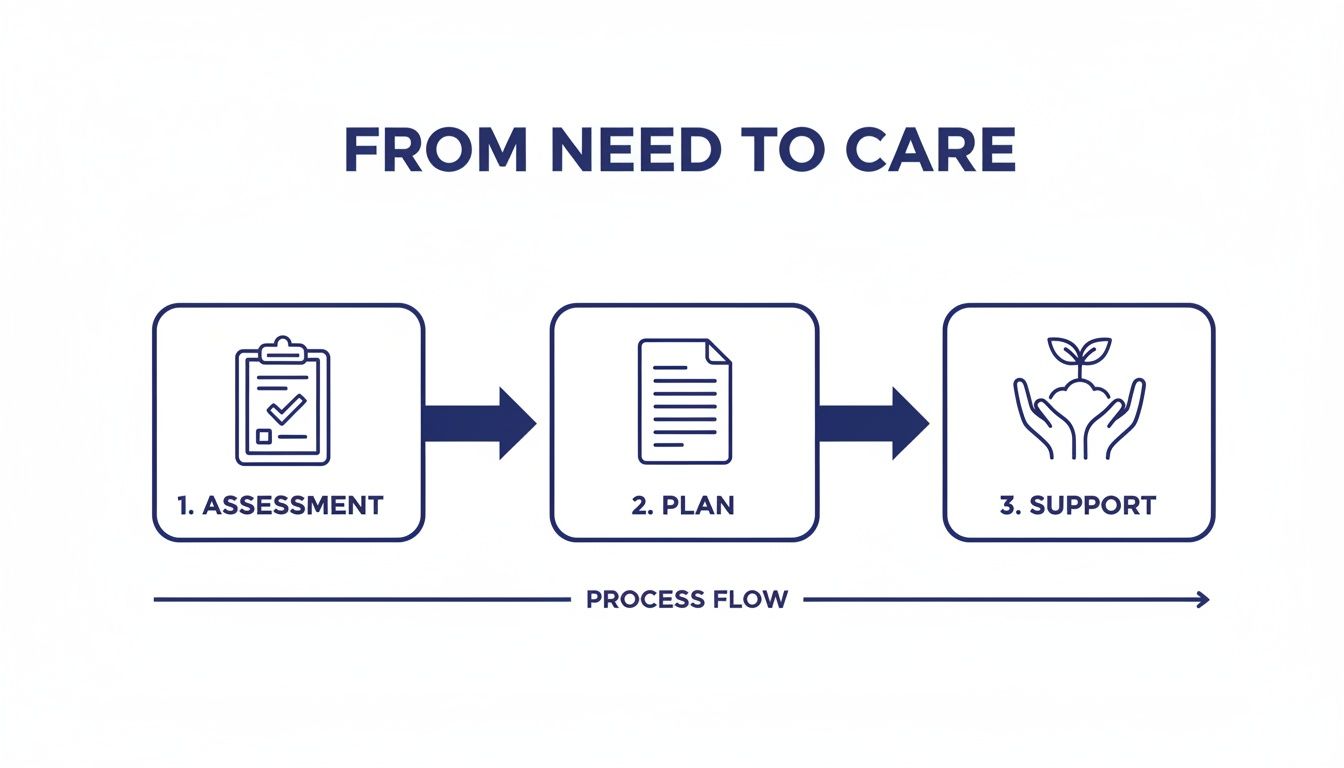
The journey from figuring out what you need to actually getting that care follows a clear path. A thorough assessment creates a solid plan, which then becomes the foundation for getting the right team in place at home.
Bringing Your NDIS Plan to Life
So, what does this look like in the real world? Let’s imagine ‘Alex’, who lives in Western Sydney and has complex respiratory needs that require ventilation support at home.
- The Plan: Alex gets his first NDIS plan. It includes significant funding in his Core Supports budget to cover both his daily personal care and the specialised nursing he needs.
- The Team: He brings a Support Coordinator on board. Think of them as a project manager for his plan. They help Alex understand his funding, find registered providers like us, and get service agreements sorted.
- The Provider: Alex’s Support Coordinator connects him with a registered NDIS provider who can supply both trained support workers for his personal care and registered nurses for his clinical ventilation needs.
- Plan Management: Alex opts to have a Plan Manager handle the financial side of things. This means a third party pays his provider invoices directly from his NDIS funds, taking all that admin work off his plate.
A well-structured NDIS plan is your roadmap. Your Support Coordinator is your navigator, and your chosen providers are the vehicle that helps you reach your destination of greater independence and wellbeing at home.
Making your NDIS plan work for you starts with clearly explaining what you need. When you have your planning or review meetings, go in prepared. Bring letters and reports from your GP or specialists that detail exactly why you need both personal and clinical supports at home. For more tips, check out our guide on how to prepare for your NDIS planning meeting. A little preparation goes a long way in ensuring your plan truly reflects your needs and gives you the power to live safely and confidently at home.
How to Choose the Right Disability Home Care Provider in Sydney

Choosing a partner for your disability home care services is one of the biggest decisions you’ll make. This isn’t just about hiring someone to handle a few tasks; it’s about inviting a team into your home and putting your health, wellbeing, and personal space in their hands.
The right provider becomes a true ally—someone who works alongside you to hit your goals and genuinely improve your quality of life. Sydney has a lot of providers, each with different specialties and ways of working. Your mission is to find the one that doesn’t just have the right clinical skills but also clicks with your family’s personality and communication style. Taking the time to ask the right questions upfront will save a world of stress later on.
Creating Your Provider Checklist
Before you even think about picking up the phone, it helps to get a crystal-clear idea of what you’re looking for. A little structure can turn an overwhelming search into a manageable one. Think of yourself as an interviewer looking to fill a very important role.
Start by listing your non-negotiables. These are the absolute must-haves. Then, create a list of your “nice-to-haves”—the qualities that would make a provider the perfect fit.
Your essential checklist should cover these key areas:
- Credentials and Registration: Is the provider fully registered with the NDIS? This is the baseline, ensuring they meet national quality and safety standards.
- Staff Qualifications: What kind of training and qualifications do their support workers and nurses have? Get specific and ask about their experience with your particular health needs. For example, ask, “Are your nurses trained in managing PEG feeds?”
- Care Planning Process: How do they actually create a care plan? It absolutely must be a team effort where your input isn’t just welcome—it’s essential. For instance, do they ask what time you prefer to wake up and have meals?
- Communication and Updates: Who will be your main point of contact? How often will you get updates, and what’s the protocol for emergencies? A practical question is, “If our regular support worker calls in sick, how and when will we be notified?”
Asking the Right Questions During Your Search
Once you have a shortlist, it’s time to dig deeper. A conversation—whether on the phone or in person—is where you get a real feel for whether a provider’s promises match their practice.
Let’s picture a family in Campbelltown searching for disability home care for a loved one. They need complex wound care and help with daily personal tasks. To compare providers fairly, they’d ask each one the same set of sharp, focused questions.
Questions about Clinical Expertise:
- Can you tell me about your nurses’ specific experience managing chronic or complex wounds like ours?
- How do you ensure there are no gaps in care if our regular nurse is sick or on leave?
- What is your process for spotting and responding to signs of infection or other complications?
Questions about Personal Support:
- How do you match support workers with clients based on things like personality and preferences?
- What’s your training process for getting new staff up to speed on our family member’s specific routine and communication needs?
- How do you handle feedback or concerns if we have an issue with a support worker?
A provider’s answers to these questions tell you so much more than just what they can do. They give you a window into their company culture, their real commitment to person-centred care, and how much they value open, honest communication.
This methodical approach lets the Campbelltown family compare apples with apples. Maybe Provider A has the most skilled wound care nurses, but Provider B offers more flexible scheduling. Additionally, provider C could be the standout for its amazing communication, guaranteeing a weekly check-in call from a dedicated care coordinator.
By writing down the responses, the family can make a confident decision based on facts, not just a gut feeling. It’s a huge step, and finding a team that delivers both clinical excellence and real compassion is what matters most. To see what a professional framework for care looks like, you can learn more about how a provider like Core Nursing Solutions structures its services to prioritise safety and dignity.
Ultimately, this decision is about finding a partner you can trust to put your family’s wellbeing first, day in and day out.
Ensuring Quality and Dignity in Disability Home Care
Great disability home care isn’t just about ticking boxes or clinical tasks. It’s built on a bedrock of safety, dignity, and a genuine respect for you as a person. This is where the official rules meet real-world compassion, creating an environment where you feel secure, heard, and truly valued.
Every family deserves the peace of mind that comes from knowing there are clear protections in place. In Australia, the NDIS framework provides a strong structure to make sure these standards are not just met, but lived and breathed by providers, giving you confidence in the support you receive at home.
The NDIS Watchdog: Your Safeguards
Think of the NDIS Quality and Safeguards Commission as the national watchdog for the disability sector. They’re the independent body that sets the rules and makes sure every registered provider sticks to them. Therefore, their job is to protect your rights and hold providers accountable for the quality and safety of their care.
From the Commission come the NDIS Practice Standards. These aren’t just bureaucratic documents; they’re the practical blueprint for what good, safe support looks like day-to-day. For instance, they cover everything from how medication is managed safely to how your privacy is protected and how your feedback is handled. When a provider has truly woven these standards into their daily work, it shows a deep, non-negotiable commitment to your wellbeing.
Quality care is proactive, not reactive. It’s about spotting a potential risk long before it becomes a problem and already having a plan to manage it. That foresight is what separates a good provider from a great one.
From Rules on a Page to Safety in Your Home
So, how do these standards actually keep you safe? Let’s look at a real-world example, like managing seizures.
A proactive provider doesn’t just wait for an emergency to happen. For someone living with epilepsy, their team would:
- Work together with you, your family, and your neurologist to create a detailed Seizure Management Plan. This plan would include practical steps like what position to place you in and when to call an ambulance.
- Train every support worker not just on the plan, but on how to spot the subtle, person-specific triggers and early warning signs that you know best. For instance, a particular sound or a feeling of dizziness might be an early sign.
- Document every seizure with precision—time, duration, type—to provide vital feedback to your medical team. This helps the neurologist make informed decisions about medication adjustments.
- Regularly review the plan with you to make sure it’s still working and adapts as your needs change.
This same hands-on approach applies across the board. A skilled nurse might notice the very early signs of a urinary tract infection, like minor confusion or a slight change in behaviour. By flagging it with a GP immediately, they can prevent a serious illness and a potential trip to the hospital. It’s this clinical watchfulness that makes all the difference.
More Than Just Tasks: Upholding Your Dignity
Beyond the safety plans and clinical skills lies the human side of care. Upholding dignity means that your independence, your choices, and your personal values are respected in every single interaction. It’s about seeing you, not just a diagnosis.
This is never more important than during sensitive conversations, like end-of-life care planning. A compassionate provider guides these discussions with empathy, ensuring your wishes are clearly documented and will be honoured. They support the family to create an environment that respects cultural beliefs and personal values, helping to bring comfort and peace during a difficult time. For example, they might ensure specific religious rituals can be performed or that a favourite piece of music is played.
Ultimately, choosing a home care provider is about finding a partner. You need someone who will champion your right to live safely and with dignity, respecting everything from how you like your morning coffee to your most deeply held beliefs. Your care should be a reflection of who you are.
Building a Collaborative Care Team for Better Outcomes

Exceptional disability home care isn’t delivered in a silo. The best results always come when your provider acts as the central hub, bringing your entire support network together for a seamless care experience. It’s a team sport where everyone—from your GP to your physiotherapist—works in concert.
Think of your disability home care provider as the conductor of an orchestra. Each specialist, like your speech pathologist or occupational therapist, is an expert in their part. The conductor’s job is to make sure they all play in harmony to create something beautiful—which, in this case, is your holistic wellbeing.
This collaborative approach is absolutely essential for managing complex needs and hitting your personal goals. It keeps everyone on the same page, sharing crucial information and working towards one unified plan.
Coordinated Care in Action
Let’s look at a real-world example. Imagine someone at home is navigating mobility challenges after a stroke and also dealing with dysphagia (swallowing difficulties). If everyone works separately, you risk conflicting advice and serious safety issues.
A collaborative care team, on the other hand, creates a much safer and more effective support system:
- The in-home nurse connects directly with the speech pathologist to understand the exact food textures and safe swallowing techniques needed, making sure every meal is supportive and safe. A practical outcome is a chart in the kitchen clearly showing which fluids need thickening.
- That same nurse also liaises with the physiotherapist, reinforcing prescribed exercises and mobility strategies during daily personal care routines. For example, they might prompt the person to do specific leg-strengthening exercises while sitting in their chair.
- Every update and observation gets communicated back to the client’s GP, giving the primary doctor a complete, real-time picture of their health. To illustrate, this could be a quick email noting a slight increase in blood pressure readings over the week.
This integrated approach means safer mealtimes, better mobility, and fewer trips to the hospital. To get a closer look at how skilled nurses make this happen in the community, you can explore the details of community nursing and its central role in coordinated care.
Supporting the Whole Family
It’s so important to recognise the massive contribution of family carers. They are often the absolute backbone of the support system, putting in countless hours of unpaid care. Professional disability home care is designed not just to support the individual, but to strengthen the wellbeing of the entire family.
The goal of professional home care is to work in partnership with the family. We provide expert clinical support while also offering that vital respite, allowing family carers to recharge and avoid burnout.
The pressure on unpaid carers in Australia is immense. A recent survey revealed a sharp drop in their wellbeing, with only 15.3% reporting very good or excellent health, compared to 43.8% of the general adult population. On top of that, 58.8% of these carers found it hard to find high-quality respite services. You can see more insights in the full 2025 Carer Wellbeing Survey report.
By bringing in a professional team, you introduce skilled support for complex tasks and give family members a chance to step back, confident that their loved one is in safe, capable hands. This could be as simple as having a support worker come for a few hours so a family carer can go to a doctor’s appointment or just have a coffee with a friend. This balance is the key to sustainable, long-term care at home.
Frequently Asked Questions About Disability Home Care
Stepping into the world of disability home care can feel overwhelming, and it’s natural to have questions. We hear a lot of the same queries from families across the Sydney region, so we’ve put together some straightforward answers to help clear things up.
How Quickly Can Services Start?
This is one of the first things people ask, and the answer is often faster than you might think. A quality provider can typically have support in place within a few days to a week after your initial assessment.
The first step is always a consultation where we get to know you and understand your needs. From there, we create a care plan and find the right support staff for you. In urgent situations, this can all be fast-tracked. For example, if someone is being discharged from the hospital, we can work directly with the discharge planner to make sure care is ready the moment they walk through the door.
Can We Choose Our Support Workers?
Yes, absolutely. This is your home and your life, and feeling comfortable with the person supporting you is non-negotiable. A person-centred approach means you are at the heart of every decision, including who provides your care.
Most providers will arrange a ‘meet and greet’ so you can see if the personality and approach of a potential support worker is a good fit. For example, if you are a quiet person who enjoys reading, you might prefer a support worker with a calm demeanour over someone who is very chatty.
The right match goes far beyond just skills on paper. It’s about finding someone you connect with, someone you can trust and feel respected by. Your preference should always be the priority.
What Happens If Our Needs Change?
Life isn’t static, so your care plan shouldn’t be either. A good provider understands this and will schedule regular reviews—usually every few months or whenever there’s a big shift in your health or circumstances. This keeps your support relevant and effective.
Let’s say you’ve been doing physiotherapy and have regained some mobility. Your personal care plan can then be adjusted to focus more on building on that independence, rather than providing full physical help. A practical change might be reducing hands-on showering assistance to simply having someone on standby for safety. The key is open communication. If you ever feel your needs are changing, let your provider know. If you have questions about adjusting your care plan, we encourage you to get in touch with our team to talk through your specific situation.
Pingback: Discover service agreement template ndis for Complex Care - Core Nursing Solutions
Pingback: Understanding NDIS Reportable Incidents: A Guide to Qualifying and Reporting - Core Nursing Solutions
Pingback: Assistance with Daily Life NDIS: Your Complete Guide - Core Nursing Solutions
Pingback: Understanding Home Care Services Cost in Sydney - Core Nursing Solutions
Pingback: Home Care Services Sydney (home care services sydney): How to Choose a Provider - Core Nursing Solutions
Pingback: Chronic illness management for NDIS: Build a strong care plan - Core Nursing Solutions
Pingback: Finding the Right Home Health Care in Sydney - Core Nursing Solutions