Picture this: a highly skilled health professional, providing expert medical care, right in the comfort of your own home. That’s the heart of modern home health care. A genuine partnership that brings clinical excellence into the familiar, reassuring space of your daily life. For instance, instead of travelling to a clinic for a complex dressing change, a registered nurse performs the procedure in your living room.
Why Home Health Care Is a Partnership in Wellbeing
It’s best to think of home health care like an active collaboration. Imagine having your own personal ‘health concierge’. Such as professionals who work with your GP, specialists, and allied health team to make sure your care is connected. By utilising this approach, it is absolutely vital for bridging the gap between being discharged from hospital and truly living independently again. A practical example is a nurse coordinating with a hospital discharge planner to ensure a patient’s home is equipped with the right medical supplies before they even arrive home.
For so many families across Sydney, this model is a game-changer. This is because it provides an alternative to facility-based care. In this case, allowing people with complex medical needs to get top-tier clinical support without giving up their place in the community. This includes many NDIS participants, aged care participants and private clients.
The Growing Need for Home Health Care Clinical Support
The demand for high-quality clinical support at home is skyrocketing. In fact, projections for 2025 show a massive shortfall in available Home Care Packages in Australia. While over 530,000 people are expected to need home care, only 299,765 packages will be funded. That leaves a staggering 230,000 individuals potentially without the support they desperately need.
This gap shines a spotlight on the critical role of specialised providers who can deliver expert in-home nursing care. It underscores the importance to find a team that offers consistent, reliable, and expert care when the wider system is so stretched. This kind of reliability is the bedrock for successfully living independently with a disability.
Home health care empowers people by bringing the clinical standards of a hospital into the comforting environment of the home.
A Focus on Dignity and Independence
At the end of the day, the true value of home health care is its deeply personal, human-centred approach. This is because it all comes back to a simple belief: everyone deserves to live with dignity, no matter what health challenges they face.
So, what does this look like in practice?
- Customised Care Plans: A registered nurse sits down with you and your family to map out a plan that fits your specific NDIS goals. For example, a care plan might detail specific strategies for managing blood sugar levels so an individual with diabetes can confidently attend a weekly art class.
- Flexible Scheduling: Care is organised around your life, not the other way around. This could be as simple as scheduling medication support to fit in before you head out to meet friends. For a university student, this might mean a nurse visit in the early morning for catheter care, leaving them free for lectures and study sessions.
- Familiar Surroundings: Getting complex care like wound management or ventilation support at home minimises the disruption and stress that clinical settings often create. As an example, child needing overnight respiratory support can sleep in their own bed, instead of an unfamiliar hospital room.
This collaborative model completely shifts the dynamic. Thus, becoming a partnership you actively guide which paves the way for better health and a richer quality of life.
What Kinds of Services Are Actually Involved in Home Health Care?
When you hear “home health care,” it’s easy to picture someone just helping with daily chores. But in reality, it’s a whole spectrum of skilled clinical services that bring professional, personalised care right into your living room. It is much more than basic support. Moreso, it is about turning a familiar space into a centre for managing complex health needs with dignity and expertise.
To make sense of it all, services are usually grouped by the level of need they address. This helps everyone understand what’s possible, whether it’s managing medical equipment or getting help with the fundamentals of daily living.
Think of home care as the central hub connecting you, your GP, and the hospital. This connection ensures everyone is on the same page, creating a truly collaborative care network.
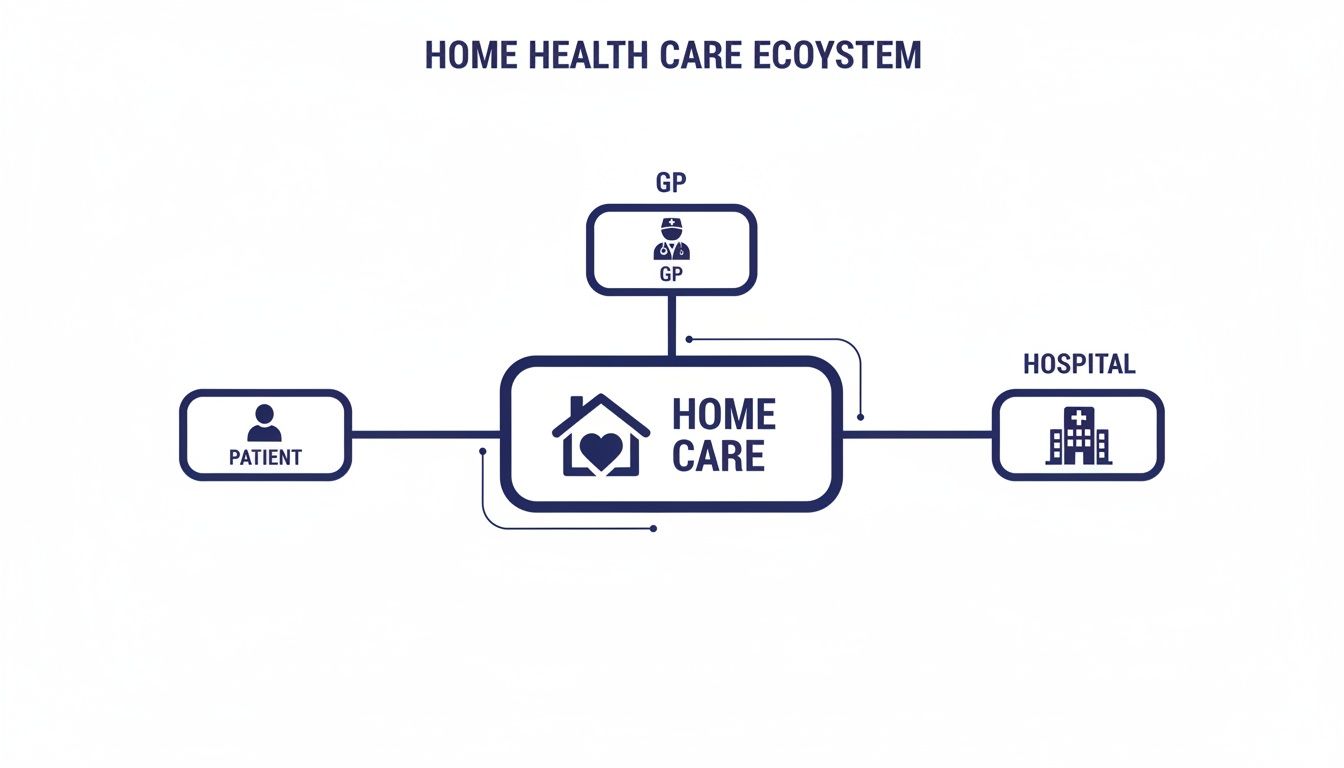
As you can see, professional home health care isn’t an isolated service. Rather, it is a vital link that fosters clear communication and teamwork across a person’s entire health support system.
Advanced Medical Support Home Health Care
For someone with really intensive health needs, this is the level of care that makes living at home a safe and viable option. In this case, tasks that would typically require a hospital stay, all managed by highly trained registered nurses.
A perfect example is tracheostomy care which Involves keeping an airway clear, performing suctioning, and changing dressings. Such critical jobs that demand clinical precision to prevent infection and ensure someone can breathe safely. For example, a nurse conducting a dressing change for a tracheostomy tube and teaching a family member how to spot early signs of an issue.
Ventilation support is another essential service in this category.
- CPAP/BiPAP Management: Our nurses make sure the equipment works flawlessly, the mask fits comfortably to avoid pressure sores, and the settings are just right for effective respiratory support. For example, a nurse might adjust the humidifier setting on a BiPAP machine to prevent a client’s airways from drying out overnight.
- Non-Invasive Ventilation (NIV): For those with more significant breathing challenges, nurses constantly monitor oxygen levels and breathing, adjusting the equipment in partnership with respiratory specialists to keep things stable. To illustrate, a nurse might take hourly oximeter readings and report them to a specialist to fine-tune ventilation pressures remotely.
This is the kind of high-level care that allows NDIS participants with profound disabilities to stay in their communities, surrounded by loved ones, instead of living in a clinical facility.
Proactive Management of Chronic Conditions
Lots of people live with ongoing health conditions that need consistent, skilled oversight to sidestep complications. Home health care provides that proactive support, helping individuals stay well and avoid those stressful, last-minute trips to the hospital.
At its heart, managing a chronic condition at home is all about empowerment. Our nurses provide expert clinical care and practical education, giving individuals and their families the confidence to handle health challenges themselves. Ultimately, leading to better long-term health and a much higher quality of life.
One of the most frequent needs we see is complex wound care.
- Post-Surgical Wounds: After an operation, a registered nurse can manage complicated dressings, watch for any signs of infection, and make sure everything heals as it should. To illustrate this, a nurse visiting daily to clean and redress a wound from a hip replacement, measuring its progress and sending photo updates to the surgeon.
- Diabetic Ulcers: For people with diabetes, specialised foot and wound care is crucial for preventing serious complications, including amputations. This could involve a nurse using a special debridement technique on a foot ulcer and fitting an off-loading boot to promote healing.
Administering injectable medications is another common task. A nurse can manage injections for conditions like diabetes (insulin) or multiple sclerosis, ensuring the dosage and technique are spot-on while also teaching family members how they can safely help. For example, a nurse could set up a weekly pre-filled syringe schedule for a client with arthritis who struggles to draw up their own medication. Our team is highly skilled across a wide range of disability home care services designed for these exact situations.
To help you see the full scope of what’s available, this table breaks down the different types of services, with clear examples of how they help.
Home Health Care Services At a Glance
| Service Category | Specific Examples of Care | Who It Helps |
|---|---|---|
| Advanced Clinical Care | Tracheostomy management, invasive and non-invasive ventilation support (CPAP/BiPAP), seizure monitoring. | Individuals with profound disabilities or complex respiratory conditions who require hospital-level care at home. |
| Chronic Condition Management | Complex wound care (e.g., diabetic ulcers, post-surgical wounds), injectable medication administration, catheter care. | People managing long-term health issues like diabetes, MS, or recovering from surgery, aiming to prevent complications. |
| Daily Living & Personal Support | Enteral (PEG) feeding assistance, complex bowel and continence management, mobility support with clinical oversight. | NDIS participants and individuals needing help with daily activities due to their medical condition, ensuring safety and dignity. |
This table shows just how flexible home health care can be, adapting to support a huge range of needs, from the most medically intensive to the more personal.
Personalised Assistance for Daily Living
Finally, home health care often blends clinical supervision with personal assistance. This is where our trained support workers, guided by registered nurses, step in to help with daily activities that have become challenging due to a health condition.
This is about more than just a helping hand. It’s about providing support with a deep clinical understanding of the person’s specific health needs.
Example of Some Clinical Support You Can Receive at Home
- Enteral Feeding Support: For those who get their nutrition through a tube (PEG feeding). Support workers can manage the feeding schedules while nurses oversee the tube site and maintenance. For example, a support worker setting up a feeding pump for a scheduled overnight feed, ensuring the rate is correct as per the dietitian’s plan.
- Complex Bowel and Continence Care: Can involve catheter management and developing consistent bowel routines. These are supervised by a nurse to ensure everything is handled safely and with dignity. For instance, a support worker might assist a client with a spinal cord injury with their daily bowel care program, following a specific nurse-developed protocol.
- Epilepsy and Seizure Monitoring: Our trained staff can provide daily support while staying alert for any seizure activity, ready to follow a management plan developed by the clinical team. This could involve a support worker who is trained to recognise pre-seizure indicators accompany a client to the park.
Who Truly Benefits from Home Health Care Nursing?
The real power of home health care comes to life in the day-to-day reality of the people it supports. It’s far more than just a list of clinical services; it’s a lifeline that helps people maintain their independence, gives families peace of mind, and strengthens the entire support network.
When you look at real-world situations, you start to see who really reaps the rewards of this personalised approach to care.
Think about an NDIS participant in the Sutherland Shire who needs ventilation support to breathe. The alternative might be living long-term in a clinical facility. Instead, specialised in-home nursing allows them to stay at home surrounded by family and plugged into their local community.
Nurses are there to manage the complex equipment, monitor respiratory function, and provide the high-level clinical oversight. This is demonstrated by taking a complex medical need and making it a manageable part of daily life.

This is what person-centred care is all about: adapting clinical expertise to fit someone’s life, not forcing them to fit their life around a clinical setting.
Empowering Individuals and Families
For families, the impact is just as significant. Imagine a family in Wollondilly caring for a child with epilepsy. The constant worry about when the next seizure might happen can be completely exhausting, both mentally and physically.
Bringing in trained support workers and registered nurses who know how to provide specialised seizure monitoring and management offers an incredible sense of security. This support means the family can finally take a breath, knowing their loved one is in safe, capable hands. For example, having a trained support worker allows the parents to go grocery shopping together for the first time in months, confident that their child is being watched over by someone who knows exactly what to do. Importantly, this helps prevent caregiver burnout and keeps the whole family unit stronger.
The goal of in-home nursing isn’t just to treat a condition. The aim is to enhance the quality of life for everyone involved. Fundamentally, it builds a circle of support that empowers participants, reassures families, and creates a stable, predictable care environment.
This collaborative approach is especially important for those navigating long-term health issues. You can learn more about how our expert teams help with these ongoing challenges by exploring our guide to chronic condition management.
A Vital Partner for the Wider Health System
The positive effects of home health care ripple out far beyond the individual’s front door. Such care creates a more efficient and effective healthcare system by becoming a key partner for other medical professionals.
- For General Practitioners (GPs): A reliable home nursing team essentially becomes the GP’s eyes and ears in the home. Our nurses can monitor a patient’s condition between appointments, provide real-time updates on things like wound healing or medication side effects, and flag potential problems before they escalate. For instance, a home care nurse might notice a patient’s blood pressure is consistently high and send a detailed report to the GP, prompting a medication review before the next scheduled appointment.
- For Hospital Discharge Planners: That transition from hospital back to home is a critical time. That is why a professional home care provider ensures that discharge is safe and seamless, dramatically reducing the risk of complications or readmissions. As a practical example, a home care provider can confirm that a hospital bed has been installed and oxygen tanks are ready at a patient’s home before the hospital finalises the discharge.
- For NDIS Support Coordinators: When a participant has high-quality clinical care locked in at home, it gives their support coordinator immense confidence. Ideally, this would involve helping the participant achieve their broader NDIS goals, like building skills or getting more involved in the community. For example, with clinical care managed, a support coordinator can focus on enrolling their client in a TAFE course they’ve been dreaming of.
In every case, home health care serves as that crucial connecting piece, fostering clear communication and teamwork across the entire care network.
Real-World Scenarios in Sydney
Let’s bring it home with another practical example. An elderly man in Picton is recovering from major surgery and needs complex wound care to avoid a nasty infection. Without in-home nursing, he’s facing either frequent, painful trips to a clinic or a much longer, undesirable hospital stay.
Instead, a registered nurse visits him right at home. The nurse not only changes the dressings using proper sterile techniques but also takes the time to teach the man and his wife how to spot the early signs of infection. This proactive care helps prevent a hospital readmission, saves the healthcare system money. Most importantly allows him to recover with dignity in the comfort of his own home.
These stories all point to a simple truth: home health care is about so much more than just medical tasks. Home health care is about enabling people to live their best, fullest lives, no matter what health challenges they face. This foundation creates a powerful ripple effect across communities. For one thing, participants gain more independence and families find that much-needed reassurance.
Navigating NDIS Funding For Your Home Care
Figuring out the funding for home health care can feel like the biggest challenge, but it doesn’t have to be a nightmare. For NDIS participants across Sydney, a bit of insight into how the system works can make all the difference. The real secret is drawing a clear, undeniable line between your clinical needs and your NDIS goals.
When you’re getting ready for a plan meeting or a review, just saying you need a nurse isn’t enough. You have to connect the dots for the planner.
Think of it this way: needing help with enteral feeding isn’t just a medical task. It’s what allows you to maintain your health and energy, which in turn helps you achieve your NDIS goal of ‘Improved Daily Living’ by being able to get out and participate in the community. To clarify, clearly explaining that link is absolutely crucial to getting the right funding in your plan. For instance, you could say, “With a support worker to manage my PEG feeding, I can volunteer at the local library, which helps me meet my goal of community participation.”
Your Support Team in the NDIS System
The good news is, you’re not in this alone. The NDIS has two key roles specifically designed to help you make sense of your plan and find the right people to deliver your supports. Therefore, knowing who they are and how a provider like us works with them is the key to a smooth journey.
- Plan Managers: These are your NDIS financial experts. This is because they take the stress out of managing your budget by handling all the invoices and paying your providers for you. In retrospect, this frees you up to focus on your care, not the paperwork.
- Support Coordinators: Think of a support coordinator as your personal guide to the NDIS world. Their job is to help you unpack your plan, track down the best providers for your unique clinical needs, and get those services up and running. We have strong relationships with support coordinators across the Sydney-to-Wollondilly area, making sure they know exactly what our nurses can do so they can confidently connect us with the right clients.
This collaborative approach makes sure your clinical needs are perfectly matched with a skilled provider, and the funding flows exactly as it should to cover those services.
Securing the right support is all about building a strong case. It means gathering the right evidence to clearly show how specialised in-home nursing is both reasonable and necessary for you to achieve your personal NDIS goals.
Gathering Your Essential Documents
To get the funding you need, you have to back up your request with solid proof. Your NDIS planner needs to see official documentation from medical professionals that confirms your clinical needs.
Here’s a practical checklist of what you should start gathering:
- Hospital Discharge Summaries: These are gold. They outline your medical condition, the treatment you received, and, most importantly, the official recommendations for your ongoing care at home. For example, a summary might explicitly state “Requires daily wound care by a Registered Nurse for the next 4 weeks.”
- Allied Health Reports: Assessments from your occupational therapist, physio, or speech pathologist provide expert, third-party validation of your support requirements. For instance, an OT report might recommend specific manual handling equipment and trained support staff for safe transfers.
- Letters from Your GP or Specialist: A letter that explains your diagnosis and spells out why clinical care at home is essential is incredibly powerful. For example, a neurologist’s letter might state that in-home seizure monitoring is necessary to prevent injury and hospitalisation.
- Current Care Plans: If you have any existing plans detailing your day-to-day support, share them. Ultimately, they help paint a complete and accurate picture for the NDIS.
You can get a better sense of how it all fits together by checking out our other resources on NDIS in-home care. Having these documents ready to go for your planning meeting will make a world of difference.
Private Funding and Other Pathways
While the NDIS is a major source of funding, it’s not the only way to get care at home. Many people choose to fund their home health care privately. This route offers complete flexibility and control, allowing you to arrange services immediately without needing to meet NDIS eligibility criteria. It’s a common path for those waiting for an NDIS plan to be approved or for individuals whose needs fall outside the scheme.
The need for quality home-based support is huge. With Australia’s aged care system supporting 1.3 million people and over 95% of seniors wanting to stay in their own homes, the demand is clear. The waiting list for Home Care Packages hit 68,586 by June 2024, which shows just how vital both NDIS and private options are.
Whether it’s through the NDIS, a Home Care Package, or private funding, the objective is always the same: getting you the high-quality care you need to live independently and safely at home.
How to Choose the Right Home Care Provider

Choosing a home health care provider is a huge decision, one that directly impacts your safety, your independence, and your quality of life. This isn’t just about hiring a service; you’re inviting a care team into your home and putting your trust in their hands.
With so many options across Sydney, it’s easy to feel overwhelmed. But the right provider will feel like a true partner—someone who works with you, your family, and your doctors. To find them, you need to look past the glossy brochures and get to the heart of what they offer: their people, their processes, and their commitment to you.
Clinical Expertise and Staff Qualifications
The bedrock of great care is the skill of the team. Therefore, the nurses and support workers walking through your door must be suitably qualified, registered, and have hands-on experience with your specific health needs. This isn’t just a detail; it’s a non-negotiable for your safety.
Don’t be shy about asking for credentials. This is about making sure the team has the real-world skills to manage complex tasks. Whether it’s tracheostomy care, ventilation support, or anything in between.
Here are a few questions to get the conversation started:
- Are all your nurses currently registered with the Australian Health Practitioner Regulation Agency (AHPRA)?
- What specific training and experience do your staff have with my condition (e.g., complex wound care, seizure management)?
- How do you keep your team’s skills sharp with ongoing training and professional development? For example, do they attend annual workshops on new ventilation technologies?
A trustworthy provider will welcome these questions and be proud to show you how qualified their team is.
Person-Centred Care Planning
Exceptional care is never a one-size-fits-all script. It should be built around your goals, your preferences, and your life. This is what we call a person-centred approach, and it’s the hallmark of a provider who genuinely cares. You should always feel like you are at the centre of every decision about your health.
This should be obvious from your very first conversation. A good provider will ask about you as a person, not just about your diagnosis. They’ll want to know what you hope to achieve—whether that’s having enough energy to see friends or managing your health so you can keep enjoying a favourite hobby.
A great care plan is a living document, not a static checklist. It should be co-created with you and your family, reviewed regularly, and adapted as your needs or goals change. This collaborative spirit ensures the care you receive is always relevant and empowering.
Ask potential providers how they plan to involve you. You could ask, “How will you work with my family to create and review my care plan?” or “How do you make sure my personal preferences are respected in the day-to-day routine?” For example, you might ask, “If my goal is to attend my grandson’s Saturday soccer games, how would the care plan support that?” Their answers will tell you everything you need to know about their commitment to putting you first.
To help you through this process, we’ve put together a checklist of essential questions. Think of it as a guide to help you compare providers and find the best fit for your needs.
Essential Questions to Ask a Home Health Care Provider
| Area of Evaluation | Key Questions to Ask | What to Look for in the Answer |
|---|---|---|
| Staff & Expertise | Are your nurses AHPRA-registered? What experience do they have with my specific condition? How do you handle staff training? | Look for confidence and transparency. They should be able to provide clear details on qualifications, specific experience, and ongoing education. |
| Care Planning | How will you involve me and my family in creating my care plan? How often is the plan reviewed and updated? | The answer should focus on collaboration. They should describe a process where you are the central decision-maker and the plan evolves with you. |
| Safety & Emergencies | What are your procedures for a medical emergency? How do you ensure infection control in the home? | You want to hear about clear, established protocols. They should be able to walk you through their emergency response and safety measures. |
| Communication | Who is my main point of contact? How can I reach them after hours? How do you communicate with my GP or other specialists? | A strong answer will detail a clear communication chain, including after-hours support and a collaborative approach with your broader medical team. |
| NDIS & Accreditation | Are you a registered NDIS provider? Are you a member of any industry bodies like ACIA? | "Yes" is the simple answer you're looking for. This confirms they meet national quality and safety standards. |
Asking these questions will give you a much clearer picture of a provider’s values and capabilities. Ultimately, helping you make a choice built on confidence and trust.
Safety and Quality Standards
When it comes to home health care, nothing is more important than safety. A provider’s official credentials and memberships are a direct reflection of their commitment to high standards and being held accountable. They aren’t just logos on a website; they show a promise to follow industry best practices.
In the Sydney area, there are two key credentials to look for:
- Registered NDIS Provider: This is a must for any NDIS participant. It proves the provider meets the strict quality and safety benchmarks set by the NDIS Quality and Safeguards Commission.
- ACIA Membership: Membership with the Aged & Community Care Providers Association (ACIA) shows a provider is serious about upholding high industry standards for private community nursing.
Beyond these, ask about their internal safety rules. Questions like, “What’s your process if there’s a medical emergency?” or “How do you handle infection control at home?” are completely fair and essential to ask. For example, you could ask, “What specific steps do your staff take to prevent cross-contamination when managing my catheter” For a better sense of what a quality provider can offer, take a look at our overview of home care services in Sydney.
Ultimately, making the right choice comes down to building a foundation of trust. The journey starts with knowing you are in safe, qualified, and caring hands.
Your Questions About Home Health Care Answered
Deciding to bring a care team into your home is a big step, and it’s completely normal to have a few questions. The goal here is to give you that last bit of clarity you need to feel confident moving forward.
How Flexible Is Scheduling?
This is usually one of the first things people ask, and rightly so. The short answer is: care schedules should be built entirely around your life, not the other way around. Proper home health care isn’t a rigid, nine-to-five service. It is designed to fit seamlessly into your routine, your family’s rhythm, and your personal goals.
Think of it this way: an NDIS participant in Campbelltown might just need someone for a couple of hours in the morning to get ready for a community program. Meanwhile, someone in the Sutherland Shire recovering from surgery might need a nurse to pop in for several short visits throughout the day for wound care and medication.
A good provider will sit down with you to map out a schedule that actually works. This might look like:
- Overnight support for someone who needs seizure monitoring or help with a ventilator.
- Quick, daily visits for administering injectable medications.
- Longer shifts to give a family carer a much-needed break (respite).
It all comes down to flexibility. The care plan is there to support your life, not dictate it.
What Happens in a Medical Emergency?
This is a crucial question, and one every professional provider must have a rock-solid answer for. Your safety is always the number one priority. Before any care starts, the clinical team should develop a detailed emergency plan with you and your family.
The emergency plan is an individual plan that outlines exactly what to do in different situations. Furthermore, it must include your medical history, current medications, emergency contacts, and clear instructions related to your condition.
In an emergency, our staff are trained to respond quickly and calmly. The first priority is always immediate safety and calling for emergency services (000) if required. Right after that, our team gets in touch with the designated family members and provides a full report to your GP and our own clinical management team.
For example, if a person living with epilepsy has a seizure that goes on longer than usual, the support worker on shift knows the exact steps laid out in the care plan—like when to administer emergency medication and precisely when to call an ambulance. Having this all planned out ahead of time removes any guesswork, ensuring a fast, effective response when it matters most.
Will I Have the Same Carers Consistently?
Building a genuine, trusting relationship with the people who come into your home is absolutely essential. That’s why any good provider will focus on creating a small, consistent team of nurses and support workers just for you. This continuity of care isn’t just a “nice-to-have”; it’s incredibly important.
For one, it means your team gets to know you properly—your unique needs, your preferences, and even your communication style. Especially because they are the ones who will notice the subtle changes in your health that a stranger might easily miss.
It also helps build real trust and a strong personal connection. It just feels better and safer having familiar, friendly faces around.
Here’s a practical example:
Imagine an elderly woman in Wollondilly who needs complex wound dressings. Having the same registered nurse for each visit means that nurse knows the wound’s history inside and out. They can spot the tiniest sign of infection and have already built a rapport that makes an often uncomfortable process that much easier for her. Of course, things like staff holidays or sickness can happen, but the goal is always to keep your core team as consistent and reliable as possible.
At Core Nursing Solutions Pty Ltd, we believe in providing clear answers and exceptional care. If you have more questions or you’re ready to talk about what you need, our team is here to help you create a personalised plan for you.
Find out how we can support you by visiting us at https://corenurses.com.au.

Pingback: Palliative Care Home Care A Guide to Compassionate In-Home Support - Core Nursing Solutions
Pingback: Private Nurse at Home: Compassionate In-Home Care for Your Family - Core Nursing Solutions
Pingback: Your Complete Guide to a Home Nursing Service in Sydney - Core Nursing Solutions