When you hear “NDIS in home care,” what comes to mind? For many, it’s about getting the right kind of clinical and personal support without having to leave the comfort and familiarity of home. Funded through your National Disability Insurance Scheme plan, it’s a way for people with permanent and significant disabilities to live with greater independence, choice, and dignity.
This isn’t about fitting into a pre-made system; it’s about building a system that fits you.
What NDIS In Home Care Actually Means

Trying to manage complex health needs on your own can feel like an impossible task. From coordinating appointments to handling daily clinical tasks, it can be completely overwhelming. NDIS in home care steps directly into this challenge. It’s not just about getting a bit of help; it’s about having the right support delivered by skilled professionals in the one place you feel most comfortable—your own home.
Think of it as bringing hospital-level expertise right to your doorstep, seamlessly blended with the routines of your daily life. Instead of constant trips to a clinic, specialised care comes to you. For example, a person recovering from major surgery might need daily wound dressing changes. Instead of travelling to a medical centre, an NDIS-funded nurse can perform this task at their bedside, reducing stress and promoting faster healing. This entire approach is built on a simple but powerful idea: your home is often the best environment to manage your health and well-being.
A Modern Approach to NDIS in Home Care Personalised Support
In the past, care models were often rigid, sometimes forcing people into residential facilities to get the support they needed. NDIS in home care turns that idea on its head. It’s fundamentally person-centered, which means your support plan is designed around your unique goals, your preferences, and your lifestyle.
What does that look like in the real world? It could be a registered nurse providing overnight ventilation support so someone with complex respiratory needs can sleep safely at home with their family. For another person, it might be daily assistance with personal routines—like showering, getting dressed, or preparing meals—that gives them the confidence to start their day right. A practical example is a young adult with an intellectual disability who wants to learn to cook simple meals. Their NDIS in home care worker can come to their home twice a week to guide them through recipes, helping them build skills and independence in a familiar kitchen.
This shift towards community-based support has been massive. The NDIS has driven huge growth in the sector, which is projected to include around 21,734 provider businesses by 2025. This explosion is a direct response to the strong demand for home-based services, showing a nationwide move toward empowering people in their own communities.
The Core Components of NDIS In Home Care
At its heart, NDIS in home care is a partnership. A good provider works closely with you, your family, and your doctors to map out a care plan that is both structured and flexible. This collaboration ensures everyone is on the same page and that the support you receive truly works for you. While similar in some ways, it’s a very different model to other government programs, like the Commonwealth Home Support Program (CHSP).
To give you a clearer picture, here’s a quick breakdown of what makes up NDIS in home care.
Core Components of NDIS In Home Care at a Glance
This table summarises the essential elements of NDIS in home care, providing a quick reference for participants and families.
| Component | Description | Examples |
|---|---|---|
| Clinical Nursing Care | Medical support delivered by registered or enrolled nurses, guided by your GP or specialist. | Wound management, medication administration (including injections), catheter care, tracheostomy support. |
| Personal Care | Hands-on assistance with daily self-care tasks to promote hygiene, comfort, and independence. | Help with showering, dressing, grooming, mobility support, and mealtime assistance. |
| Complex Support | Specialised, high-intensity care for participants with significant health needs requiring specific training. | Enteral (tube) feeding, ventilation support (CPAP/BiPAP), complex bowel care, seizure management. |
Ultimately, these components come together to create a support network that allows you to live safely and confidently on your own terms.
Unlocking NDIS Funding for Home Support
Trying to figure out if you or a loved one qualifies for NDIS in home care can feel a bit like wading through mud. The official guidelines can be dense, but once you break them down, the core requirements are actually quite clear. Getting a handle on these criteria is the essential first step to getting the support you need at home.
At its heart, the NDIS is there for Australians living with a permanent and significant disability. To be eligible, you’ll need to tick a few key boxes. Think of these as the main checkpoints on your journey to getting funding.
The Three Main Eligibility Checks for NDIS in Home Care
It’s helpful to think of NDIS eligibility as a three-legged stool. If one leg is missing, it won’t stand up. You generally need to meet all three of these conditions to get into the scheme.
- Age Check: You need to be under 65 when you first apply for the NDIS. If you’re 65 or older, the support system you’d look to is typically My Aged Care.
- Residency Check: You must be an Australian citizen, hold a permanent visa, or be a Protected Special Category Visa holder. You also have to be living in Australia.
- Disability Check: This is the big one. You need to have a disability that is both permanent (lifelong) and significant.
That last point—”permanent and significant”—is where most of the questions come up. It’s not just about having a medical diagnosis; it’s about how that condition genuinely impacts your ability to go about your day.
So, What Does ‘Significant Disability’ Really Mean?
When the NDIS says ‘significant’, they’re talking about how much your disability affects your day-to-day life. Do you need help from another person to get things done? Do you rely on special equipment just to manage?
A ‘significant disability’ is one that seriously affects your ability to manage key areas of your life, like getting around, communicating with others, looking after yourself, or being part of your community. It means you need ongoing help to do things that others might not think twice about.
Take, for example, someone with a progressive neurological condition. Their disability is ‘significant’ because it might make it impossible to get around their house safely, cook a meal, or handle personal care without assistance. A practical example is a person with multiple sclerosis who experiences severe fatigue and muscle weakness. They might need a support worker to help them shower and dress in the morning so they have enough energy to go to work or attend a community group in the afternoon. They need consistent NDIS in home care to maintain their independence and quality of life.
Building a Strong Case for Your Application
When you apply, the National Disability Insurance Agency (NDIA) needs proof that you meet these criteria. Your application is your chance to tell your story and clearly show why you need support. This is where gathering the right paperwork becomes so important.
A solid application is backed by reports and letters from professionals who know you and your condition well.
Here’s a Real-World Example:
Let’s think about Ben, a young man with cerebral palsy that affects his movement and coordination. To secure funding for personal care at home, his family would gather evidence like:
- A letter from his neurologist confirming his diagnosis is lifelong.
- An occupational therapist’s assessment that details exactly how Ben needs physical help with showering, dressing, and preparing food.
- A physiotherapist’s report that explains the specific supports he needs to move safely within his own home.
This collection of documents does more than just name a condition; it paints a clear picture of why Ben needs NDIS in home care to live his life. By focusing on how the disability affects daily function and backing it up with professional evidence, you can confidently work through the application process and get one step closer to the right support.
Making Sense of Your NDIS In Home Care Funding
When you first get your NDIS plan, figuring out the funding for NDIS in home care can feel a bit like trying to read a foreign language. It’s easy to get lost in the details. The best way to get your head around it is to stop thinking of it as one big pile of money.
Instead, picture your NDIS plan as three separate bank accounts. Each account is set aside for a very specific purpose, and once you know what each one does, you’re well on your way to making your plan work for you.
Decoding Your NDIS Funding Budgets
For the kind of support you need day-to-day, your most important budget is almost always going to be Core Supports. This is the flexible funding designed to help you with everyday life and kick your personal goals.
- Core Supports: This is your account for daily living. It covers all the practical help you might need, like personal care, help with household chores, and support to get out and about in your community. Most of the funding for nursing and personal assistance comes straight from here.
- Capital Supports: Think of this as your fund for equipment and technology. It’s for those bigger, one-off purchases that make a huge difference, like assistive tech, modifying your home with a ramp, or getting a specially-equipped vehicle.
- Capacity Building Supports: This budget is all about investing in you. It’s designed to fund things like therapy, training, or support coordination that help build your skills and independence over the long haul.
Tucked inside your Core Supports budget is a really important category called ‘Assistance with Daily Life’. This is the engine room of your home care plan—it’s where the funds for services like personal care, medication management, and in-home nursing are specifically kept.
Before you can get a plan, however, you need to be eligible for the NDIS. The infographic below breaks down the three main pillars the NDIS looks at.
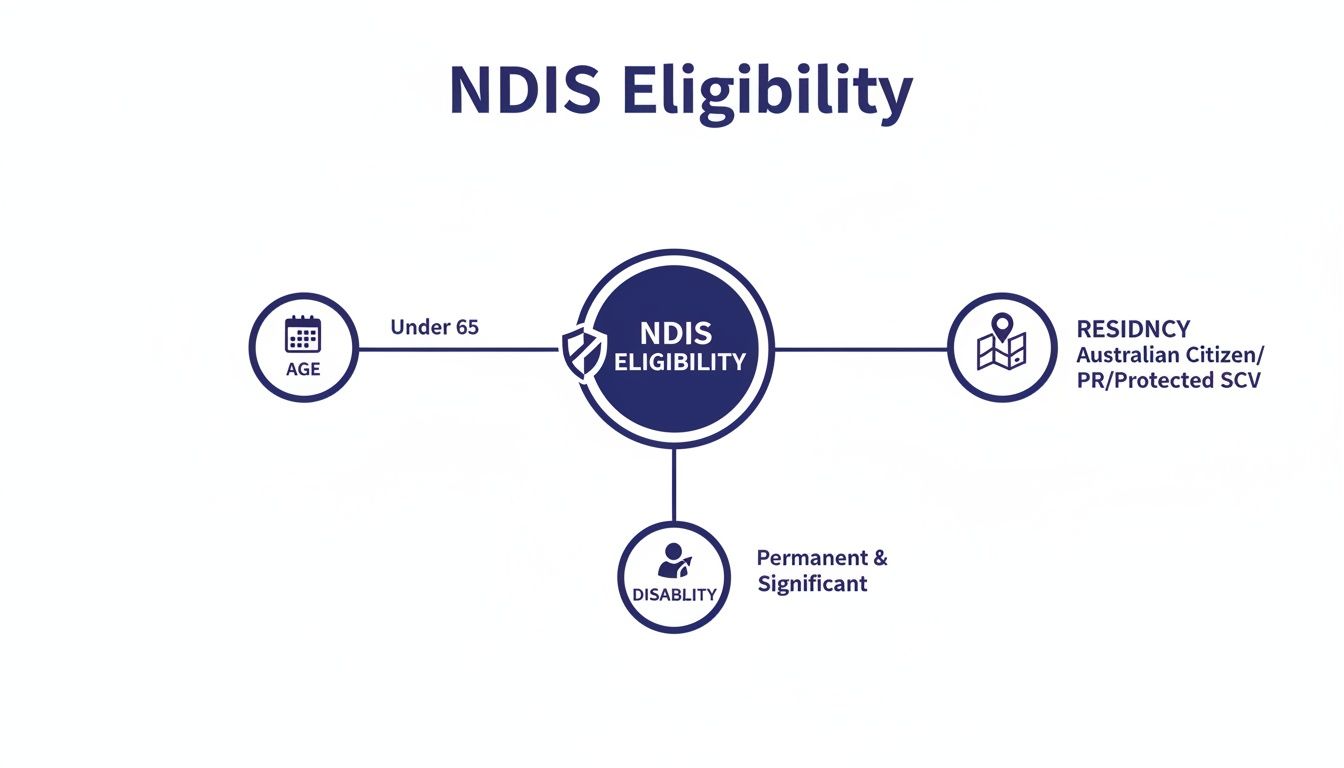
As you can see, access to NDIS funding all starts with meeting specific age, residency, and disability requirements. Once those are confirmed, a plan can be created.
How You Can Manage Your NDIS Funding
Once your plan is approved, you get to decide how the money is actually managed. This is a big decision, as it changes how you pay providers and how much direct control you have over your budget. There are three main ways to go about it.
Choosing how to manage your NDIS funds is about finding the right balance between control, flexibility, and administrative support. Your choice should reflect what makes you feel most confident and empowered.
Let’s break down what each option looks like in the real world.
1. Self-Management
You’re in the driver’s seat. The NDIA deposits the funds directly into your bank account, and you’re responsible for paying your providers’ invoices yourself. This gives you maximum flexibility and lets you use both registered and non-registered providers.
- Practical Example: Sarah self-manages her plan. After her support worker finishes their shift, they send her an invoice. Sarah simply transfers the payment from her bank account and keeps a copy for her records.
2. Plan Management
Think of a plan manager as your financial go-between. They’re a separate organisation that takes care of paying your providers on your behalf, using your NDIS funds. You get the same flexibility as self-management but without the paperwork.
- Practical Example: David uses a plan manager. His in-home nurse sends invoices straight to the plan manager, who pays the bill from David’s NDIS plan. The manager tracks all the spending, leaving David free to focus on his health.
3. NDIA-Managed (Agency-Managed)
With this option, the National Disability Insurance Agency (NDIA) handles everything. They pay your providers directly from your plan. It’s the most hands-off approach, but the trade-off is that you can only use NDIS-registered providers.
- Practical Example: Emily is NDIA-managed. Her provider, a registered nursing service, logs into the NDIS portal after each visit and claims their payment directly. Emily doesn’t have to touch a single invoice.
The good news for participants is that the government is continuing to invest heavily in these supports. In 2023-24, social benefits spending jumped 15.5% to $167.2 billion, a rise driven largely by disability services. The NDIS is set to spend $46.2 billion this year, with an extra $175.4 million allocated over the next four years to ensure the scheme delivers safe and high-quality NDIS in home care. You can learn more about these government finance statistics and what they signal for the future of disability support in Australia.
What Kind of NDIS In Home Care Support Can I Get?

So, you understand the basics of NDIS funding. The next big question is, what does that translate to in real life? What kind of help can you actually get at home?
NDIS in home care isn’t a single, rigid service. It’s a broad spectrum of support that can range from a little help with daily routines to round-the-clock clinical care. The whole system is designed to be flexible and meet you exactly where your needs are.
Think of it like building blocks. Some people just need the foundational block of personal care. Others need to add community nursing on top, and some require highly specialised, high-intensity support. Understanding what’s available helps you pinpoint what you need to live safely and independently at home.
The Foundation: Personal Care and Daily Assistance for NDIS in Home Care
This is often the first and most fundamental layer of NDIS in home care. It’s all about the everyday tasks that many people take for granted, but which can be a real challenge for others. This support is about more than just ticking off a to-do list; it’s about creating a routine that upholds dignity and fosters independence.
For some, it’s the key to starting the day feeling confident and prepared. For others, it’s about conserving energy so they can get out and engage with their community later on. When a skilled support worker takes care of these tasks, it frees you up to focus on what truly matters to you.
Common supports in this category include:
- Personal Hygiene: Help with showering, dressing, grooming, and managing continence.
- Mealtime Support: Assistance with preparing healthy meals, managing dietary needs, or help during mealtimes.
- Mobility Assistance: Support with moving safely around the house, transferring from a bed to a chair, or using mobility aids.
Getting these fundamentals right is crucial for maintaining overall health and well-being. To get a better sense of how this works, you can learn more about Assistance with Daily Life under the NDIS.
The Next Level: Community Nursing Care
When your needs start to involve more clinical tasks, NDIS in home care steps up. This is where community nursing, delivered by qualified Registered or Enrolled Nurses, comes into play. These services cover medical needs that require professional training but can be safely managed right in your own home.
This layer of support is vital for people managing chronic conditions, recovering from a hospital stay, or working to prevent health complications. It effectively bridges the gap between your GP’s office and your living room, making sure your clinical care plan is followed to the letter.
Community nursing brings professional healthcare into the comfort and familiarity of your home. It’s about being proactive with your health, avoiding unnecessary hospital visits, and empowering you with the knowledge to manage your own care.
Here’s a practical example: Maria has type 2 diabetes and a complex wound on her leg. A community nurse visits her three times a week to clean and redress the wound, check for infection, and monitor her blood sugar levels. The nurse also explains Maria’s medication, helping her feel confident managing it on her own. This consistent, professional care helps Maria heal properly and keep her diabetes under control—all without leaving her home.
High-Intensity Supports for Complex Clinical Needs
At the most specialised end of the spectrum, you’ll find high-intensity supports. These are for NDIS participants with significant and complex health issues that require advanced clinical skills, specialised training, and constant oversight. These are often life-sustaining supports where precision and expertise are non-negotiable.
The ability to provide this level of care at home is a massive win for the NDIS. It means people with even the most complex conditions can live with their families and stay connected to their communities. It all hinges on a highly trained team working hand-in-glove with your doctors and specialists.
To really understand what this looks like, here are a few real-world examples:
Tracheostomy Management: Liam breathes using a tracheostomy tube. A registered nurse visits daily to provide essential care, including suctioning to clear his airway, cleaning the site to prevent infection, and changing the inner cannula. The nurse also empowers Liam and his family by teaching them to recognise early warning signs.
Overnight Ventilation Support: Sarah relies on a BiPAP machine to help her breathe at night. Her NDIS in home care plan includes an active overnight shift, where a trained support worker stays awake in her home. They monitor the ventilator, ensure the mask fits correctly, and are ready to respond instantly if an alarm sounds or if Sarah needs to be repositioned.
Enteral (Tube) Feeding: For someone unable to eat or drink, tube feeding is a lifeline. A nurse can manage this at home by administering a special nutritional formula through a PEG tube. This involves flushing the tube, programming the feeding pump, and watching for any signs of complication, like skin irritation or digestive issues.
These high-intensity supports show just how personalised and sophisticated NDIS in home care can be, ensuring everyone receives safe, effective, and dignified care at home.
Comparing NDIS In Home Care Support Levels
To make it even clearer, let’s break down the key differences between these support levels. Seeing them side-by-side can help you identify which category best fits your or your family member’s needs.
| Support Type | What It Involves | Example Scenario |
|---|---|---|
| Personal Care | Non-clinical help with everyday tasks like showering, dressing, meal prep, and moving around the house. | A support worker visits each morning to help an individual with limited mobility get showered, dressed, and have a healthy breakfast. |
| Community Nursing | Clinical tasks performed by a qualified nurse, such as wound care, medication management, and diabetes support. | A registered nurse visits a participant twice a week to manage a complex wound dressing and administer a prescribed injection. |
| High-Intensity Supports | Specialised, often life-sustaining clinical care for complex needs like ventilation, tube feeding, or tracheostomy care. | A specially trained team provides 24/7 care for a person who relies on a ventilator, including overnight monitoring and emergency response. |
Ultimately, the goal of the NDIS is to provide the right level of support—not too little, not too much. Understanding these distinctions is the first step toward building a plan that truly works for you.
How to Choose the Right NDIS Provider

Choosing a provider for NDIS in home care is probably one of the biggest decisions you’ll make on this journey. It’s so much more than just picking a name off a list; it’s about finding a true partner in your care, someone who gets you and respects what you want to achieve.
This relationship has to be built on a foundation of trust, genuine expertise, and a shared vision for your well-being. A great provider doesn’t just show up to do a job—they work with you. They listen, they adapt, and they empower you to live your best life, right in your own home. With so many providers out there, it really helps to have a clear plan for making that choice.
Your Essential Provider Checklist
Before signing on the dotted line, you need to ask some direct questions. This isn’t just about their credentials; it’s about making sure they are the right fit for you and your family. A provider who is confident in their service will always welcome your questions and give you straight, honest answers.
Think of this as a checklist to guide your conversations:
- NDIS Registration and Compliance: Are they an officially registered NDIS provider? Don’t be shy about asking for proof that they meet all the standards set by the NDIS Quality and Safeguards Commission.
- Real-World Experience: What is their track record with your specific health needs? Ask for examples of how they’ve supported others with similar conditions, whether it’s complex continence care or ventilator support.
- Staff Qualifications: What kind of training and qualifications do their nurses and support workers have? Do they invest in ongoing professional development, particularly for those high-intensity supports where skill really matters?
- Communication and Planning: How will they keep you and your family in the loop? What’s their process for creating a care plan, and how much say will you have in the decisions being made?
This isn’t about putting them on the spot. It’s a conversation to make sure you feel completely comfortable and secure. A transparent provider will have this information ready to go and will be happy to talk it all through with you. To get a better sense of what top-tier support looks like, have a look at these disability home care services and see the benchmark you should be aiming for.
Looking Beyond the Brochure
Let’s imagine a family trying to decide between two providers for their father, who needs daily wound care and help with his personal routine. Provider A has a flashy website and makes big promises. Provider B is smaller but has glowing recommendations from a trusted support coordinator.
The family meets with both. Provider A sends a sales rep who gives a polished but generic presentation. Provider B, on the other hand, sends their clinical nurse manager. She sits down with their father, asks about his day, what he enjoys, and what makes him feel most comfortable. She spends more time listening than talking.
The difference between an average provider and an excellent one is often found in the small details: how well they listen, how they personalise their approach, and how they make you feel seen and heard as an individual.
The family goes with Provider B. Why? Because from that very first meeting, they showed a genuine person-centred approach. They proved they were there to support a person, not just to manage a medical condition. This is the gold standard of NDIS in home care.
The Importance of Stability and Quality
The disability sector can be complex, and a 2024 national survey showed that many providers are navigating some serious financial and operational challenges. While most are incredibly resilient, it does underline how important it is to choose a stable, high-quality organisation that you can rely on to be there for you.
This is especially critical when it comes to high-acuity nursing care, where consistency and reliability are simply non-negotiable. Getting familiar with the current state of the disability sector can help you understand why locking in a dependable provider is one of the smartest moves you can make for your long-term support.
Understanding Your Rights and Safeguards in Home Care
When you invite someone into your home for NDIS in home care, your safety, dignity, and peace of mind are everything. It’s not just about getting the right clinical support; it’s about feeling respected and secure. Thankfully, strong systems are in place to protect you, and knowing your rights is the best way to feel confident about the care you receive.
The key organisation here is the NDIS Quality and Safeguards Commission. Think of them as the independent umpire of the NDIS world. Their whole job is to set the quality standards, keep an eye on providers, and step in if something isn’t right, making sure you are always put first.
The NDIS Code of Conduct in Practice
Every single registered NDIS provider and their staff must live by the NDIS Code of Conduct. This isn’t some dusty legal document; it’s a real-world promise about how you should be treated every single day.
So, what does that actually look like?
- Your Right to Privacy: Your personal details and health information are exactly that—personal. For example, a support worker should never discuss your care with anyone else, like a neighbour, unless you’ve given them clear permission to speak with a specific family member or doctor.
- Your Right to Speak Up: You should always feel comfortable giving feedback or making a complaint. A practical example is if a support worker consistently arrives late. You have the right to raise this with the provider without fearing it will negatively impact your services.
- Your Right to Be Heard: Your provider must listen to what you want. If you’ve said you’d prefer a female support worker or that you need personal care at a specific time of day, that choice needs to be respected wherever possible.
At its heart, the NDIS Code of Conduct turns the provider-client relationship into a true partnership built on trust. It gives you the power to expect—and demand—care that is all about you.
How to Provide Feedback or Make a Complaint
If you’re ever unhappy with any part of your care, there are clear steps you can take to sort it out. Your voice is important, and the system is designed to make sure it gets heard.
- Talk to Your Provider First: Often, the quickest and easiest way to resolve something is to speak directly with your provider’s management team. A good provider will have a straightforward feedback process and will genuinely want to fix the problem with you.
- Contact the NDIS Commission: If you don’t feel comfortable talking to your provider, or if you’re not happy with their response, you can take your complaint straight to the NDIS Quality and Safeguards Commission. It’s your right to do this, and they will investigate your concerns independently.
Proactive Risk Management: A Practical Example
A great provider doesn’t just wait for problems to happen; they are always thinking ahead to keep you safe.
Let’s imagine a scenario. A community nurse is visiting to give a participant their daily medication and notices they seem more tired and unsteady than usual.
Instead of just ticking the box and leaving, the nurse takes a moment. She reviews the participant’s recent medication chart and checks their vital signs. Suspecting a potential side effect, she immediately calls the participant’s GP to share her observations. The doctor advises a small adjustment to the dosage, and the nurse updates the care plan on the spot. This simple, proactive action prevents a potential fall and keeps the participant’s medication plan safe. It’s a perfect example of managing potential NDIS reportable incidents before they can become serious issues.
Common Questions About NDIS In Home Care
When you’re sorting out NDIS in home care, it’s natural to have a lot of questions. Getting straight answers is the best way to feel confident about the choices you’re making. Let’s walk through some of the things people ask us most often.
Can My Family Member Be Paid to Provide My Care?
This is a common question, and the short answer is usually no. The NDIS is set up to fund professional support services, keeping them separate from the informal help that families naturally provide for each other. This helps maintain healthy boundaries and makes sure you’re receiving care from people with formal training.
That said, there are very rare exceptions. If you live in a remote area with no local providers, or if you have extremely specialised needs that only a family member has been trained to handle, the NDIA might consider it. This is handled strictly on a case-by-case basis and isn’t the standard way of doing things.
What Should I Do If My Support Needs Change Suddenly?
Life happens, and sometimes your health or living situation can change in a flash. If this occurs, the very first thing you need to do is call your provider. A good provider will jump into action to reassess your needs, adjust your care plan, and make sure everyone in your support circle is on the same page to keep you safe.
At the same time, you’ll want to ask the NDIA for a plan review. To get the ball rolling, start gathering any new reports from your doctors or therapists that spell out exactly what has changed. For example, if a recent fall results in a new mobility impairment, a letter from your physiotherapist explaining the need for increased personal care hours will be crucial evidence. This paperwork is vital for getting your funding updated so your support continues to be right for you. You can learn more about how the NDIS supports ongoing health in our guide to chronic condition management.
Do I Get a Say in Which Support Worker Comes to My Home?
Yes, absolutely. It’s your home and your life, so you have the right to choose who you feel comfortable with. While things like scheduling and staff availability play a part, a quality provider will always do their best to find a nurse or support worker who’s a great match for your personality and clinical needs.
Building a solid, trusting relationship with your care team is what makes NDIS in home care truly work. Don’t be shy about sharing your preferences with your provider right from the start—it helps them find the right fit for you.
How Is Complex Overnight Care Like Ventilation Managed?
When someone needs support around the clock, the NDIS has different ways to fund overnight care. The right model really depends on how intensive your needs are, which will be outlined in your medical reports.
- An ‘active’ shift is for high-needs situations where a nurse stays awake all night to actively monitor equipment, like a ventilator, and provide immediate care. A practical example is a person with a tracheostomy who requires regular suctioning throughout the night to keep their airway clear.
- A ‘sleepover’ shift is an alternative where a support worker sleeps at your home but is on-call to help if you need them during the night. For instance, a person who may need help getting to the bathroom once or twice overnight might use a sleepover shift.
At Core Nursing Solutions Pty Ltd, our goal is to give you clear answers and expert, person-centred care so you can feel confident on your NDIS journey. If you’re in the Sydney to Wollondilly region and need specialised in-home nursing support, our team is ready to help build a plan that truly works for you. Reach out to us at https://corenurses.com.au.